Introduction
Osteoarthritis (OA), also called arthrosis, is the most common form of joint disease and one of the leading causes of chronic disability, largely due to knee and hip involvement. The World Health Organization considers OA a cause of disability in at least 10% of the population over 60 years of age1. The knees are the most commonly affected joints, and it occurs more frequently in women. During the 20th century, the definition of OA changed from “hypertrophic arthritis” to the current more common consensus definition: “OA is the result of mechanical and biological events that destabilize the normal coupling of synthesis and degradation of articular cartilage, chondrocytes, extracellular matrix, and subchondral bone”2.
The etiology of OA is multifactorial and includes genetic, metabolic, developmental, and traumatic factors. OA diseases affect all joint tissues and are manifested by morphological changes: biochemical, molecular, biomechanical, cellular and of the matrix, which produce: softening, fibrillation, ulceration, loss of articular cartilage, sclerosis and destruction of subchondral bone, osteophytes, and subchondral cysts.
When OA is clinically evident, it is characterized by joint pain, tenderness, crepitus, limited movement, inflammation, and occasional effusion without presenting systemic effects.
A multicenter group of studies developed diagnostic criteria for OA of the knees3. Currently, OA is recognized as a chronic inflammatory disease involving malalignment with progressive joint loads, instability, cartilage erosion, matrix degeneration, reduced joint space damage, ligament damage, and thickening of the subchondral bone; It is also characterized as a multiple diseases with immune and central nervous system dysfunction, which contributes to complete joint damage, progression of lesions, pain, and disability4.
Treatment of injuries caused by OA of the knees is challenging, and treatment decisions for individual injuries are problematic5. There is currently a wide range of options, ranging from conservative measures, arthroscopic surgery, bone marrow harvesting techniques, osteochondral auto/allograft, cell-based techniques, growth factors, and emerging gene therapy techniques6. Arthroscopic surgery has been used frequently for the treatment of patients with OA. Its indications are limited, and there is no evidence to suggest that it alters the disease process. However, there is a select group of patients who can obtain benefit as a result of the arthroscopic procedure in terms of pain relief and functional improvement, and with this, postpone or even avoid more complex and morbid procedures, such as osteotomies or total arthroplasty7. Arthroscopic surgery is a controversial procedure for the treatment of knee OA, and there are conflicting studies about the efficacy of arthroscopic procedures8–12. Some studies have shown satisfactory results with arthroscopic surgery for several years9,12,13–20. The efficacy of arthroscopic treatment in this pathology has been described12,21,22. In addition, other studies have reported few benefits and short duration11,23,24. There are also comparative studies that show satisfactory results in normally aligned knees and poor results in those with varus angulation22. In general, for patients with knee OA who do not respond to medical treatment, which includes physiotherapy and anti-inflammatory medication, arthroscopic surgery may be a good therapeutic option7,11,25.
There are several proposed mechanisms to explain the improvement in the arthroscopic treatment of OA. These may be due to the extraction of fragments of cartilage and lose bodies, hypertrophic synovial membrane, osteophytes and degenerative tissues; by resection of adhesions, partial meniscectomies and dilution of synovial fluid and inflammatory mediators such as cytokines or inflammatory factors that play an important role in the development of OA and even by a placebo effect26. Research studies have demonstrated symptomatic improvement by performing only joint lavage27, partial meniscectomy18 and subchondral bone microfractures or abrasions28. A comparative study of abrasion plasty, with arthroscopic debridement without abrasion, demonstrated that debridement alone produced superior results25.
Young adult patients with incipient posttraumatic OA and short-term symptoms may benefit from arthroscopic surgery to treat specifically unstable areas of meniscal injuries, loose chondral fragments, and posttraumatic intraarticular changes7,9,29. The selection of patients with OA for arthroscopic surgery depends on the mentioned factors and, additionally, on their level and expectations of physical activity, as well as their age and health condition. Other factors to consider are the possible morbidities and complications of the procedure. Arthroscopic surgery produces a lower rate of complications, minimal morbidity, and a faster return to activities of daily living when compared to major procedures such as osteotomies (tibial or femoral) or arthroplasties (unicompartmental or total). However, these treatment options are clearly indicated and accepted for selected patients with very advanced OA. Factors to consider in the decision to perform these more complex procedures include increased surgical morbidity and longer convalescence and rehabilitation times. Therefore, in selected patients, arthroscopic surgery is a good alternative that also allows postponing the performance of these procedures without “burning bridges.” Patients should be informed about the palliative and temporary nature of the procedure and the possibility of requiring another major surgery if their symptoms are not relieved.
Arthroscopy can also be performed for diagnostic purposes, to define the extent and levels of OA, detect the degenerative process early and, according to the findings, perform immediate arthroscopic treatment or define the need for other types of treatment such as osteotomies or arthroplasty.
The justifications for considering arthroscopic surgery in selected patients include the possibility of improving their symptoms and function, minimum morbidity and, additionally, being able to demonstrate the stage of the arthritic process.
The results of the majority of research studies have not allowed us to draw conclusions on the precise indications for arthroscopic treatment in knee OA. In addition, it is difficult to compare the different techniques described since their results are not always related to the magnitude of the lesions, and the success rates are highly variable. Studies also do not show that arthroscopic surgery can alter the natural history of OA or produce structural changes in articular cartilage. The elaboration of the research studies does not demonstrate unified criteria or protocols for the inclusion of patients and the classification of pathological changes.
The purpose of this study was to review the results of treatment with arthroscopic surgery in patients with knee OA, determine possible predictors of satisfaction, and assess the possibilities of improving the patient selection process to provide a better correlation between their expectations and surgical results.
Methods
This retrospective longitudinal study was conducted in the Department of Orthopedic Surgery of the ABC Medical Center. A review of 59 consecutive patients with a primary diagnosis of OA of the knees treated with arthroscopic surgery was performed. Of this group, it was possible to analyze 50 patients (51 knees, one bilateral case) with the main symptom of pain with a minimum duration of 6 months, without response to medical treatment and with compliance with the inclusion criteria. An attempt was made to contact all the patients, but only 50 (84.74%) were available or were able to complete the information for follow-up and analysis.
All patients underwent a complete medical history and physical examination.
Preoperative symptoms consisted of localized pain and tenderness, joint stiffness, locking of the knee, significant entrapment, and feeling of instability (secondary to meniscal tear or loose fragments). A total of 34 patients (35 knees: 68.62%) reported having specific mechanical symptoms: sudden exacerbation of pain, symptoms of blockage and instability, and painful popping. The average pain on the visual analog scale (VAS) was 8.8 points.
All patients had symptoms of >6 months and had been previously treated for a minimum of 6 months, in many cases by other doctors, without improvement. Medical treatments consisted of activity modification, anti-inflammatory medication (including corticosteroids), glucosamine, physical therapy, weight reduction, and viscosupplementation. Most of these patients had been seen by other orthopedic surgeons who had recommended total arthroplasties. Patients with posttraumatic OA were included.
Of the 51 arthroscopic surgeries performed on 50 patients diagnosed with knee OA, 28 were performed on female patients and 23 on male patients (one bilateral). The average age was 61 years (56-80 years). The follow-up period was 3 years.
Inclusion criteria
- Clinical and radiological diagnoses of OA.
- Symptoms with a minimum of 6 months of evolution.
- A minimum period of 6 months of preoperative medical treatment.
- Failure of medical treatment.
- Osteoarthritic changes grades 1, 2, and 3 of the
Kellgren and Lawrence classification30. - Follow-up of 3 years.
Exclusion criteria
- Ligament insufficiencies.
- Previous diagnoses of rheumatoid or metabolic arthritis.
- A period of < 6 months of evolution and medical treatment.
- Grade 4 arthritic changes of the Kellgren and Lawrence classification30.
- Treatment of chondral lesions with microfractures.
- Follow-up of < 3 years.
Preoperative radiographic studies of knees were obtained in all patients. Radiographs included weight-bearing anteroposterior (AP) and lateral views in extension and patellar views with 30 and 60°of knee flexion. The degrees of OA were evaluated by examining the AP radiographs of the knees using the Kellgren and Lawrence classification (Table 1)30. According to this classification, the following evaluations were obtained: 27 knees (52.94%) corresponded to grade 1, 17 knees (23.33%) to grade 2 and seven knees (13.72%) to grade 3. Additionally, loose osteochondral bodies were identified in 10 knees (19.60%). Patients with grade 4 OA were excluded from this study.
Table 1. Kellgren-Lawrence radiological classification
| Grade | Description |
|---|---|
| 0 | Absence of radiographic changes of OA. |
| 1 | Doubtful narrowing of joint space and possible osteophytes. |
| 2 | Definite osteophytes and possible joint space narrowing. |
| 3 | Moderate multiple osteophytes, definite narrowing of joint space, mild and subchondral sclerosis and possible joint deformity. |
| 4 | Large osteophytes, severe joint space narrowing, severe subchondral sclerosis, and definite joint deformity. |
Magnetic resonance imaging (MRI) is the most useful imaging study in patients with minimal radiographic changes and localized pain with clinical findings compatible with meniscal lesions. Degenerative meniscal tears frequently coexist with OA. Proton density, fat suppression, and gradient echo techniques are very useful in the evaluation of articular cartilage31,32.
An MRI of all the knees were performed, able to demonstrate degenerative meniscal lesions with myxoid changes in 42 knees (82.35%), meniscal tears in 46 knees (90.19%) and loose bodies in the 10 already mentioned knees.
Arthroscopic surgeries were performed in all patients, and these included different procedures: synovectomy, in the cases that presented reactive synovitis; partial meniscectomies and, in some cases, subtotal, removing only unstable fragments and maintaining the continuity of the meniscus; debridement of areas with degenerative changes and meniscus remodeling; chondroplasty with resection of unstable or loose cartilage areas, preserving stable areas; resection of osteophytes in cases of impingement; abrasion plasties; lysis of adhesions and profuse joint lavage.7,33–38 Additionally, lateral retinaculum releases33 were performed in eight knees (15.68%); intercondylar notch plasty34 in 11 knees (21.56%); subchondral bone denervation35 in two knees (3.92%) and resection of anterior tibial osteophyte36 in four knees (7.84%). In no case was it necessary to use a tourniquet.
The patients were discharged the next day, and the postoperative regimen included: cryotherapy37, analgesics, ambulation with weight bearing as tolerated, and instructions for strengthening exercises and range of motion. A total of 39 patients (76.47%) required additional physiotherapy for 6-12 weeks after surgery. There were no intraoperative or postoperative incidents.
All patients were followed up at regular intervals of 2-6 weeks for the first 3 months and then at quarterly intervals until the 1st postoperative year. Subsequently, the patients were evaluated by telephone every 6-12 months until the 3-year follow-up; pain, muscle strength, range of motion, and activity levels were examined.
During arthroscopic procedures, the grades of chondral lesions were evaluated using The ICRS classification (Table 2)38; the degrees of the lesion are defined according to their osteochondral penetration (Fig. 1). In addition, the extent of chondral lesions was evaluated using the knee cartilage lesion mapping system (ICRS)39. Six separate articular surfaces were considered, and no subdivisions were considered.
Table 2. Cartilage injury classification (IRCS classification)
| Grade | Description |
|---|---|
| 0 | Normal cartilage. |
| 1a | Superficial fibrillation or softening. |
| 1b | Superficial lacerations or fissures. |
| 2 | Lesion of < 50% thickness of the articular cartilage. |
| 3a | Lesion greater than 50% thickness of the articular cartilage up to the calcified layer. |
| 3b | Lesion greater than 50% thickness of the articular cartilage deep to the calcified layer. |
| 3c | Severely abnormal defect down to the subchondral bone. |
| 3d | Severely abnormal defect with the presence of blisters. |
| 4a | Injuries exposing the subchondral bone. |
| 4b | Lesions penetrating subchondral bone. |
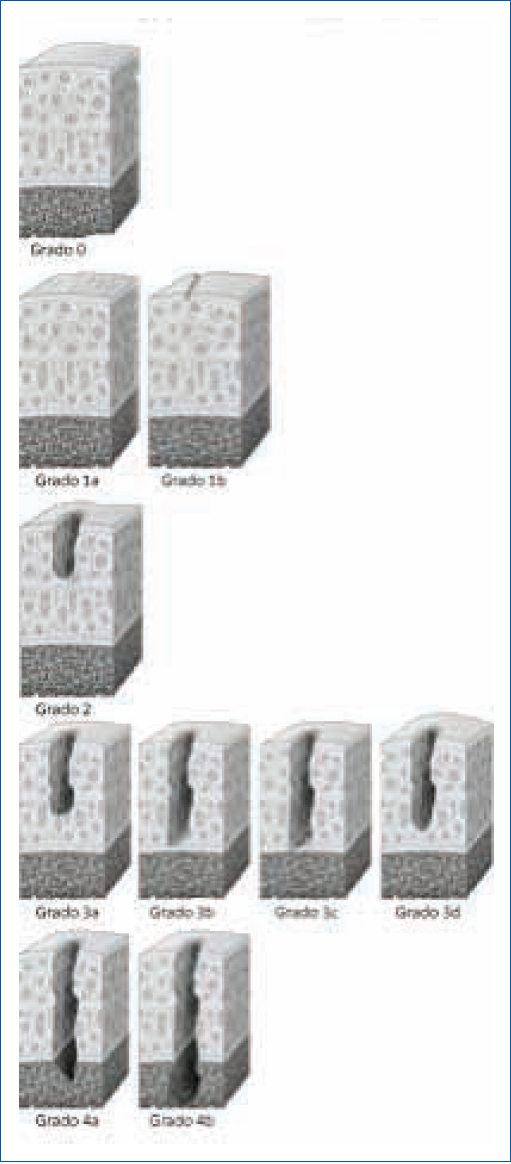
Figure 1. Cartilage injuries. Cartilage Injury Assessment System (The IRCS). Reprinted with permission from the ICRS Cartilage Injury Package. (http://www.cartilage.org/).
Thus, the extensions and penetration of chondral lesions were classified as follows:
Mild OA
Grade 1 chondral lesions and grade 2 chondral lesions on one or more articular surfaces.
Moderate OA
Grade 4 chondral lesions on one articular surface or grade 3 chondral lesions on two or more articular surfaces.
Severe OA
Grade 4 chondral lesions on two or more articular surfaces or grade 3 chondral lesions on three or more articular surfaces.
According to this evaluation (ICRS), OA was classified as follows:
- Mild OA: 10 knees (19.6%).
- Moderate OA: 30 knees (58.82%).
- Severe OA: 11 knees (21.56%).
The overall evaluation at the end of the follow-up period was carried out using a postoperative knee scale (Table 3). In this, scoring is applied considering three parameters: pain, function and range of motion40. The results are considered as good: between 9 and 12 points, regular: between 6 and 8 points, and bad: between 3 and 5 points.
Table 3. Postoperative knee scale
| Pain | |
|---|---|
| No pain | 4 points |
| Mild pain | 3 points |
| Moderate pain | 2 points |
| Severe pain | 1 point |
| Mobility | |
| Normal range | 4 points |
| Deficit of 10° or less | 3 points |
| The deficit between 10 and 20° | 2 points |
| Deficit greater than 20° | 1 point |
| Function | |
| Improvement | 4 points |
| Return to normal activities | 3 points |
| No change | 2 points |
| Worst | 1 point |
|
Results; good: between 9 and 12 points; regular: between 6 and 8 points; bad: between 3 and 5 points. |
|
Results
The general evaluation showed results as follows: good in 33 knees (64.7%), regular in 11 knees (21.56%), and bad in seven knees (13.72%).
According to the degree of severity of OA, the results were classified as follows:
- Mild OA (10 knees), moderate OA (30 knees), and severe OA (11 knees).
- Good: 7 knees (70%), good: 23 knees (76.66%), and good: 4 knees (27.27%).
- Regular: two knees (20%), regular: five knees (16.66%), and regular: four knees (36.36).
- Bad: one knee (10%), bad: two knees (6.66%), and bad: four knees (36.36).
Degenerative meniscus lesions were identified in 46 knees (90.19%). Additionally, medial meniscus tears were demonstrated in 22 knees (43.13%), lateral meniscus tears in 13 knees (25.49%) and tears of both menisci in 11 knees (21.56%). Subtotal meniscectomies (>50% meniscus) were performed in seven knees (four medial and three lateral), and partial meniscectomies (±30% meniscus) in 39 knees; trying to preserve as much tissue as possible. No tears were demonstrated in five knees (9.8%), and did not require meniscal procedures.
A total of 34 patients (35 knees-68.62%) reported having specific mechanical symptoms, including: locking, the feeling of instability, and painful clicking. In 18 of these knees, unstable meniscus tears were demonstrated; in 10 knees, loose osteochondral bodies were demonstrated; and in seven knees, combined lesions were demonstrated that, in combination, contributed especially to causing joint locking. In general, 32 of the 35 knees had good results, and this shows that 91.42% of the patients who manifested joint locking responded satisfactorily to the procedure. Results for these knees were specifically correlated as good.
In six patients (seven knees = 13.72%), the evolution had poor results; in the postoperative period, these patients required treatment with anti-inflammatory drugs, including steroids and strong analgesics. In these patients, in addition to OA, it was possible to measure, radiologically and clinically, varus alignment (greater than 6°) in four knees and valgus alienation (greater than 8°) in three knees. In three of the seven knees, the arthroscopic findings corresponded to grade 3 of the Kellgren-Lawrence radiological classification.
As a whole, the group of patients improved the mean pain score: from 8.8 to 2.9 points on the VAS and it was considered that 44 patients (86.27%) had significant improvement.
Discussion
OA is the most common rheumatologic and orthopedic musculoskeletal disorder41. Knowledge about the natural history of knee OA is scarce; however, it is known that its evolution produces different pathological changes that include: meniscus tears, chondral damage, loose bodies, osteophyte formation, mechanical malalignment and soft tissue contracture42.
In Mexico, the general prevalence of OA is 10.5% (11.7% in women and 8.7% in men), and the states with the highest prevalence are Chihuahua (20.5%), Nuevo León (16.3%), and Mexico City (12.8%)43.
The role of arthroscopic surgery in the treatment of patients with OA of the knees is highly controversial9,11. There are different arthroscopic techniques to treat lesions caused by OA, and depending on the pathology of its presentation, the appropriate surgical procedure is determined. There are also other surgical procedures for patients with knee OA that do not improve with medical treatment; these include osteotomies and total arthroplasty42. Diverse opinions have been described about the efficacy of arthroscopic surgery in the treatment of OA of the knee. In general, OA has a poor clinical prognosis even without the coexistence of mechanical alterations. However, most research studies have not demonstrated a consensus on the role of arthroscopic surgery in the treatment of knee OA, and many treatment studies do not consider subgroups of knees that define the extent of OA. On the other hand, the results of several studies have shown, in general terms, that a large percentage of knees with OA have a good clinical response to treatment with arthroscopic surgery17,20,36,44.
The results of a research study demonstrated a clinical improvement of 80% (in 32 of 40 knees) at 12 months postsurgery and 59% (19 of 32 knees) at 60 months45. However, this study is considered highly controversial since knee OA is predominant in female patients, among other differences, so its results are considered very difficult to extend to the general population46,47. Additionally, no subgroup analyses were performed in that study to determine whether there were patients who might have benefited from arthroscopic surgical treatment.
We consider the group of patients defined in our study as representative of the general population of patients with knee OA, and we also believe that our observations are internally valid and are also extendable to the general population. We tried to minimize bias in the study design as follows: susceptibility bias was minimized by including consecutive patients, and the condition was well-defined to include only tibiofemoral OA. We minimized performance and execution biases as all surgeries were performed by a single surgeon with experience in arthroscopic surgery. Transfer bias was eliminated by having no rate of patient loss during the study. The group of patients, as a whole, had an improvement in pain with an average decrease of 8.8-2.9 points on the VAS. Of the total number of patients, 44 (86.27%) had considerable improvement, which allowed them to recover their activity levels prior to the onset of their symptoms. These results are consistent with those reported in the general literature, but with the small number of patients studied, we did not observe demographic, clinical, or physical characteristics associated with the results.
The symptoms and physical signs of OA of the knee are too non-specific to predict results, and the possible presence of inflammatory disease could confuse the diagnosis of another pathology48. In a series of 154 patients with symptomatic OA of the knees and 49 asymptomatic control patients, 140 (91%) of the patients with OA had meniscal tears; however, the relationship between meniscal lesions and symptoms was not conclusive49. In our study, we demonstrated meniscus tears in 46 knees (90.19%) out of a total of 51 knees. The results of this study demonstrated that patients with mechanical symptoms had better than average postoperative outcomes; however, there is little quantitative evidence of similar outcomes in the literature50,51. In another research study, significantly better results were demonstrated in patients with mechanical symptoms, although follow-up times were highly variable (between 6 and 60 months), and differences between patients with mechanical symptoms and asymptomatic patients were not reported20. The results of our study did not define the relationship between symptoms and the possible prediction of successful results.
Some research studies have attempted to describe radiological features associated with clinical outcomes of arthroscopic procedures in OA knees; however, these features are not described quantitatively17,22,51. In addition, the results of research studies have not shown a direct relationship between pain and radiological findings52,53. The analysis of our results demonstrated radiological evidence associated with specific postoperative results in knees with OA; three of the seven patients with poor results corresponded to grade 3 of the Kellgren-Lawrence radiological classification. This reflects the severity associated with clinical outcomes in severely OA knees, and therefore arthroscopic surgery should possibly not be routinely recommended for these patients; however, the extent of chondral lesions was the only indicator of clinical outcome, and these lesions could not be predicted prior to surgery. Patients whose knees were shown to have malalignment (varus-valgus) also had poor outcomes, as described above.
Patients should be warned that the clinical outcome may depend on the extent of chondral lesions identified during surgery and that their expectations of improvement should take this possibility into account48. The analysis of this study shows that the main indication for arthroscopic surgery in OA of the knees is for those patients who present mild or moderate OA. The correlation of the degree of joint lesions with the clinical results shows that the greater the degree of lesions, the worse results are obtained. Knees classified as mild OA obtained good results in 70% (seven out of 10 cases), and knees with severe injuries only obtained 27.27% good results (three out of 11 cases). It is necessary to emphasize that the best results are obtained in patients with symptoms of mechanical blockage and in patients with satisfactory alignment of the lower limbs. An important benefit of treatment with arthroscopic surgery in patients with mild or moderate OA is that it allows them to: remain active, reduce pain and functional limitations, and postpone or avoid, in many cases, major surgery such as total arthroplasty. On the other hand, it is not clear whether patients treated with arthroscopic meniscectomies have a higher risk of OA progression than patients treated without surgery54–57.
Arthroscopic surgery can also be an option for elderly patients who have an indication for total knee arthroplasty in whom, due to their health conditions and anesthetic risks, it is preferable to perform less invasive surgery.
Our study has some strengths: it was conducted at a single medical center (Centro Médico ABC, Mexico); access to almost the entire group of patients treated (86.44%); verification of a minimum of 6 months of preoperative medical treatment and reduction of biases. In addition, complete documentation was obtained from all patients included in the study, and all received the same pre and postoperative information.
This study has several limitations: it was a retrospective analysis of data collected prospectively and without a control group; therefore, it has the weaknesses of any retrospective analysis; the analysis of results was from a single surgeon at a single medical center and as such, may not be generalizable to a larger and more diverse group of surgeons; it is also limited by a small number of patients to obtain more accurate data; we did not analyze demographic characteristics such as weight and body mass indices that may have affected clinical parameters associated with the results; clinical results were compared internally between subgroups of patients; differences in patient characteristics and procedural variability might affect results; unfortunately no functional range and mobility measurements were documented as they were not available for the study; patient satisfaction data were not evaluated. Additional prospective, randomized controlled studies with larger groups of patients are required.
Despite these limitations, we believe that the results of this study can help guide the treatment of patients with knee OA who present pain and also mechanical symptoms with meniscus tears, loose bodies, and other intraarticular injuries. Our results show that arthroscopic surgery, with the procedures already described and additional physiotherapy, produces significant symptomatic and functional improvement, over a period of 3 years, in patients with mild or moderate OA of the knees. However, the intermediate nature of follow-up, in conjunction with the low rate of poor results, raises concerns about the clinical durability of the procedure. For this reason, we considered the possibility of further monitoring this group of patients to evaluate the results of this treatment in the longer term.
Conclusion and recommendations
Arthroscopic surgery has a greater chance of success in patients with mild or moderate knee OA and especially in those with evidence of mechanical components such as loose bodies or unstable meniscus lesions. Furthermore, it could also be an alternative for patients with more severe OA with evidence of mechanical injuries and for elderly patients who, due to their health conditions and anesthetic risks, could not be candidates for total knee arthroplasty, and less invasive surgery may be recommended.
This study demonstrated that arthroscopic treatment provided improvement in pain and function in 44 knees (86.27%), achieving this way that the patients recovered the levels of activity prior to the onset of symptoms.
It is important to consider that for patients with OA of the knees, arthroscopic surgery can produce temporary and not definitive results since the evidence has not shown possibilities of stopping or reversing the degenerative process or producing permanent relief. So we can only expect good and not great results because there is no cure for OA of the knee.
We believe that these observations are relevant for establishing indications for arthroscopic surgery in patients with knee OA and may be useful for conducting studies with a more rigorous experimental design.
Funding
The authors declare that they have not received funding for this study.
Conflicts of interest
The authors declare that they have no conflicts of interest.
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that no patient data appear in this article.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
Use of artificial intelligence for generating text. The authors declare that they have not used any type of generative artificial intelligence for the writing of this manuscript, nor for the creation of images, graphics, tables, or their corresponding captions.
