Introduction
Real-time endobronchial ultrasound-guided transbronchial fine-needle aspiration (EBUS-TBNA) is a minimally invasive diagnostic technique that complements flexible videobronchoscopy and allows the bronchoscopist to evaluate beyond the inner surface of the airway. The most widely used ultrasound system is the linear probe, as it provides images of lymph nodes, blood vessels, the heart, and possible tumor masses adjacent to the airway, in addition to visualizing the needle inside the studied structure1.
EBUS-TBNA consists of a probe with a convex transducer operating at a frequency of 7.5 MHz and a penetration depth of 5 cm at its tip, which scans parallel to the direction of bronchoscope insertion2. Images are obtained through direct contact of the probe with the lesion.
Using this technique, all high paratracheal mediastinal lymph node stations (2R, 2L), low paratracheal (4R, 4L), and subcarinal (7) are accessible, except for the subaortic and paraesophageal lymph nodes (5, 6, 8, and 9)3. Hilar and interlobar lymph nodes (10 and 11) are also accessible3,4. Mediastinal adenopathies that should be studied via puncture are those that on the computed tomography (CT) have an enlarged short axis (>1 cm) or that on fluorodeoxyglucose positron emission tomography (FDG-PET) show significant metabolic activity5.
Imaging modalities – primarily CT and FDG-PET-frequently used as initial staging methods, show in Yasufuku’s study6, lower sensitivity and specificity than EBUS-TBNA. Unlike modalities, EBUS-TBNA can approach lymph nodes ≤ 10 mm in size and identify neoplastic infiltration in them.
Mediastinoscopy allows for detailed examination of lymph node stations 1, 2R, 2L, 4R, 4L, and 3, and the anterior subcarinal lymph nodes7. However, it is not possible to access lymph nodes located in lymph node stations 5, 6, 8, and 97. The mean sensitivity rate of mediastinoscopy in published studies is approximately 80%, and the mean false-negative rate is around 10%. Mediastinoscopy is a highly invasive technique, requires general anesthesia, is costly, and has a rate of complications of approximately 2% up to 3%8.
The main indication for EBUS-TBNA is the mediastinal staging of lymph nodes in patients with suspected or previously diagnosed primary or metastatic lung cancer. It allows for cytological and histological evaluation of these lymph nodes, making it a minimally invasive technique for the cytodiagnosis of mediastinal lesions9.
Other clinical applications, besides the diagnosis and staging of lung cancer, include re-staging of the posterior mediastinum after neoadjuvant chemotherapy and the diagnosis of extrathoracic metastatic malignancy, mediastinal and hilar lymphadenopathy, sarcoidosis, lymphoma, tuberculosis, endemic mycoses, and mediastinal tumors10.
The prognosis of lung neoplasms is determined, among other aspects, by the stage of the disease at the time of diagnosis. Therefore, having an accurate staging diagnosis is crucial to determine the best therapeutic option for each patient.
The sensitivity rate of EBUS-TBNA in the diagnosis and staging of lymph nodes ranges goes from 85% up to 100%, and its negative predictive value from 11% up to 97.4%; specificity and positive predictive value are 100% in all cases10,11.
In appropriate patients, it is a minimally invasive procedure without risk when performed by trained personnel. Potential complications include hemomediastinum, pneumothorax, pneumomediastinum, and abscess at this level. Overall, it is a safe and well-tolerated technique. Coagulation defects related to the use of anticoagulants or antiplatelet agents should be corrected (withdrawn 5-7 days before the procedure) and a platelet count > 50,000,000 should be ensured due to the risk of bleeding. It should be delayed for, at least, 6 weeks after an acute myocardial infarction and is contraindicated in cases of unstable ischemic heart disease, arrhythmias, and severe hypoxemia12.
The objective of our study was to describe the cytological characteristics of specimens obtained via EBUS and the use of auxiliary techniques for the cytological diagnosis of mediastinal adenopathy.
Method
We conducted a descriptive, cross-sectional, observational, and retrospective study using the database of the surgical pathology department of Centro Médico ABC. The search included all patients with mediastinal adenopathy under study who were evaluated by EUS-EBUS from January 1st, 2016 through August 31st, 2018. The study included all patients with EUS-EBUS-guided aspiration biposies and excluded those with biopsies obtained via transesophageal endoscopic ultrasound. Clinical data were obtained from each patient’s electronic health record, including age, sex, previous diagnosis, and prior treatment. In all cases, a rapid evaluation of Hematoxylin and Eosin-stained smears was performed, as well as an evaluation of the cell block. In patients with a previous diagnosis of lung cancer, immunohistochemical staining with TTF1 and napsin A was performed.
Results
The study included a total of 12 patients (8 men and 4 women), with a mean age of 60 years. Among these, 6 (50%) had a previous diagnosis of pulmonary adenocarcinoma and 6 (50%) were previously healthy or had a history of another neoplasm: 1 (8%) had a previous diagnosis of malignant melanoma, 1 (8%) of esophageal adenocarcinoma, and 1 (8%) of breast cancer. Clinical data obtained are summarized in Table 1.
Table 1. General characteristics of patients
| Clinical data | n = 12 |
|---|---|
| Males, n | 8 |
| Females, n | 4 |
| Age in years, mean (range) | 60 (28-77) |
| Final diagnosis, n | |
| Malignant | 10 |
| Benign | 2 |
| Insufficient | 0 |
The final diagnosis was positive for metastasis of pulmonary adenocarcinoma in 7 (58%) patients and positive for metastasis of a non-pulmonary site in 1 (8%). In 2 patients (16.6%), immunohistochemistry was not contributory, and they presented with granulomatous lymphadenitis. One out of these 2 patients (16.6%) had an association with yeast-like structures (Fig. 1).
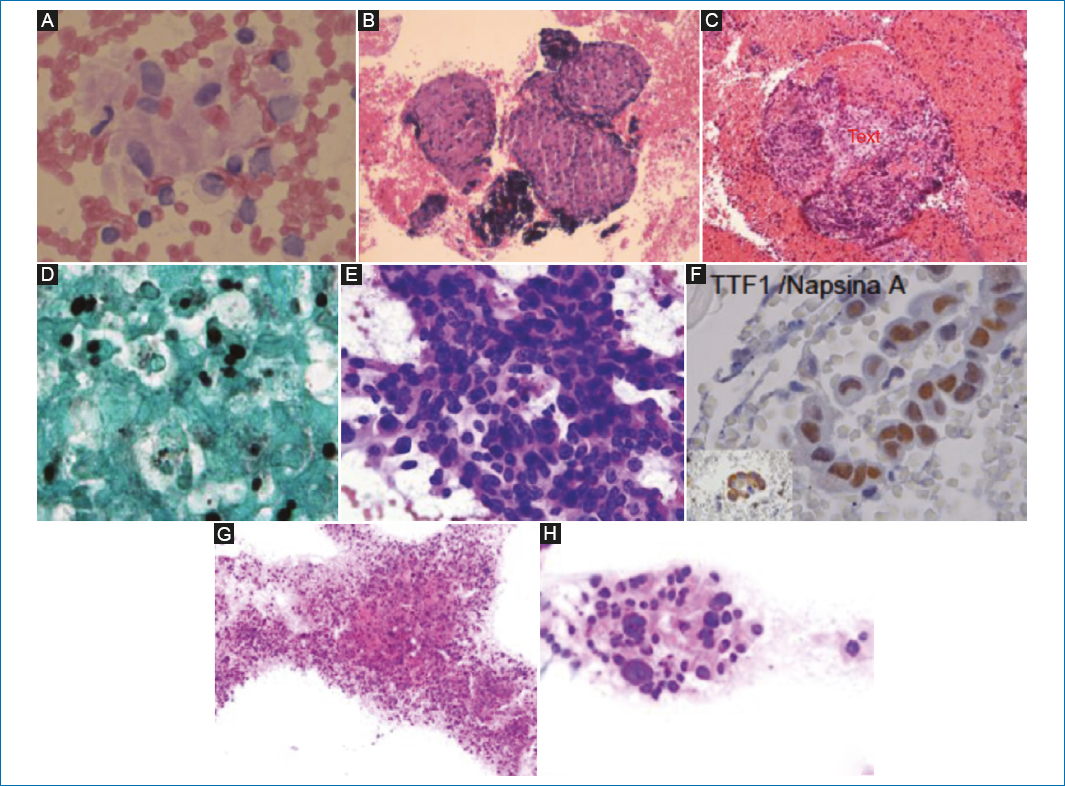
Figure 1. A: cluster of epithelial cells with ample cytoplasm. B: lymphoid nodules forming granulomas. C: necrotizing granuloma with multinucleated giant cells. D: at higher magnification, the presence of yeast consistent with Histoplasma capsulatum (GMS stain) is notable. E: the smear shows a hypercellular population with overlapping clusters of atypical cells. They exhibit atypical features, including ample cytoplasm, irregular nuclear contours, nucleomegaly, irregularity, and hyperchromasia. F: immunohistochemical reaction on the cell block shows nuclear positivity for TTF1 and napsin A (inset). G: panoramic micrograph with clusters of neoplastic cells, chronic inflammation, and necrotic tissue. H: at higher magnification, the atypical characteristics of the cells are apparent.
Discussion
EUS-EBUS has become the initial diagnostic modality for the study of mediastinal and pulmonary adenopathies. This technique represents a rapid and minimally invasive method for the staging of lung cancer. Its sensitivity rate ranges from 36% up to 96%, and specificity rate from 88% up to 100%. The advent of targeted therapy has revolutionized the treatment of lung cancer. Currently, pathologists must classify non-small cell lung carcinoma and perform molecular biology studies where possible. Using EBUS, material can be obtained in up to 98% of cases for immunohistochemical studies. There are other findings in EBUS-guided aspiration biopsies, besides neoplastic cells, including granulomas. Granulomas have been detected in 2% up to 22% of EBUS-guided biopsies. Some studies have shown that up to 5% of patients with a history of lung cancer may develop a sarcoid-like granulomatous reaction after treatment. Sarcoid-like reactions in patients with non-pulmonary neoplasms have been well documented in cases of lymphoma, gastric carcinoma, and breast cancer. Although their pathogenesis is poorly understood, it has been suggested that they represent an uncontrolled immune response to neoplasm.
Conclusions
The use of EBUS for the evaluation of mediastinal adenopathy has increased worldwide, allowing for findings other than metastases of neoplasms in these biopsies, such as granulomas. The use of histochemistry and immunohistochemical panels is of great help for a precise final diagnosis, and molecular biology studies can even be conducted in cases that warrant them.
Funding
The authors declare that they have not received funding.
Conflicts of interest
The authors declare no conflicts of interest.
Ethical disclosures
Protection of human and animal subjects. The authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of data. The authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consent. The authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Use of artificial intelligence for generating text. The authors declare that they have not used any type of generative artificial intelligence for the writing of this manuscript, nor for the creation of images, graphics, tables, or their corresponding captions.