Background
The orbit is formed by the confluence of seven bones classified into an exoskeleton (formed by external portions of the maxilla, zygomatic, and frontal bones) which form the orbital rims and an orbital endoskeleton formed by the internal wall of the lacrimal, palatine, and sphenoid bones1. Orbital floor fractures are common injuries, recorded in about 100,000 patients per year in the United States by the National Hospital Ambulatory Medical Care Survey2.
Traffic accidents are the most frequent etiology reported in the literature associated with craniofacial fractures, being the cause of 82.8% of the cases, followed by falls 11.7%, work accidents, and other causes 3% and interpersonal violence 0.7%3,4. The highest incidence occurs in men (93.1%). The maxilla is the most commonly involved in combined facial fractures (68%), followed by the mandible (32%), orbit (6.2%), and zygomatic complex (5.5%)5,6. Facial fractures are subdivided into upper third, middle third, and lower third of the face, but involvement of the midface and mandible constitutes the same principles of repair as a true panfacial fracture would dictate7.
Other authors advocate reduction and fixation of complex injuries within the first 48 h, when the initial edema has resolved. Management within the first 10 days is critical because soft-tissue stiffness and interfragmentary healing make late corrections more difficult8,9.
The sequence, timing, and materials used in orbital floor fracture reconstruction are still a matter of debate. Surgical treatment of orbital floor fractures depends on several considerations. The immediate evaluation is to assess whether or not there is entrapment of the medial or inferior rectus muscle resulting in necrosis, fibrosis, and scarring. In extreme cases, patients with entrapment may experience bradycardia, nausea, and syncope when attempting to perform extraocular movements (the oculocardiac reflex) and immediate operative reduction with release of the entrapped muscle is of immediate importance. While the most common indication for repair is the correction of enophthalmos, resulting from loss of orbital floor support. Whereas mediate consideration at 2 weeks > 2 mm enofthalmos, or > 50% orbital floor involvement, will require repair to avoid diplopia and obvious ocular asymmetry. Some authors recommend treatment within the first 72 h if the patient does not require neurosurgical management10,11.
Case Report
Male patient, 51 years old, with no significant history for the current condition, started falling on the ground, impacting the right orbital region (Fig. 1).

Figure 1. Clinical photographs of the patient.
On admission, it was decided to perform a CT scan of the facial mass with 3D reconstruction (CT) with a diagnosis of pure blow-out fracture in the right orbital floor (Fig. 2); therefore, it was decided to perform a surgical approach. It was decided to perform an open reduction with the combination of lactosorb plates, titanium mesh, and costal cartilage. We started with orotracheal intubation, proceeding with a right subciliary approach, dissecting the skin, the muscle of the orbicular fibers, the orbital septum until reaching the subperiosteal plane identifying the inferior orbital rim (Fig. 3); we continued with the desperiostization locating the orbital floor; finding the fracture of the orbital floor with herniation of the fatty tissue and the eyeball towards the ipsilateral maxillary sinus. The soft tissues are reduced and the fracture is fixed with a preformed titanium mesh with onlay technique and just above it, the lactosorb plate with anterior fixation with a 5 mm absorbable screw. After this, the 20 × 20 mm costal cartilage is placed with a convex configuration (Fig. 3). A forced duction test was performed and the result was negative. Closure in two planes is performed.
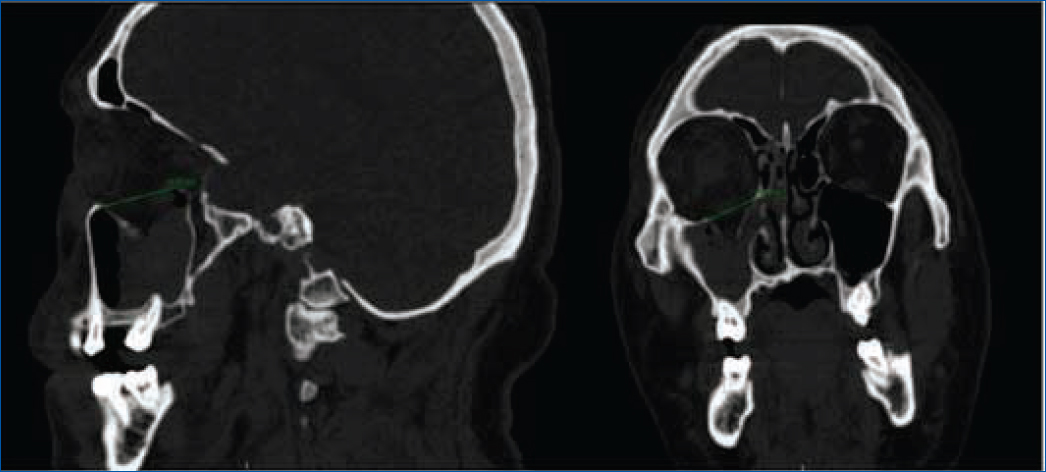
Figure 2. Pure blow-out type right orbital floor fracture; tomography in sagittal and coronal view.

Figure 3. Subciliary incision and titanium mesh.
In the post-operative period, we performed a control tomography with adequate reduction. The patient was discharged without complications with revision during the following 4 months, with no record of enophthalmos, diplopia, or dystopia (Fig. 4).

Figure 4. Post-operative result.
Discussion
In the repair of orbital floor fractures, the greatest challenge is to establish the facial framework since the trauma results in the lack of reliable bony landmarks, which if not adequately reduced produce, in addition to a post-traumatic facial deformity and post-operative functional problems.
The most common complications after surgical repair of the orbital floor are persistent postoperative diplopia, infraorbital nerve dysfunction, and enophthalmos12,13. The incidence of post-operative diplopia ranges from 20% to 52% in several published series14–16.
A review of more than 300 orbital floor repairs by standardized post-operative anthropometry revealed an overall ectropion rate of 2.6% in operated eyes, significantly higher than the rate in non-operated eyes and no significant increase in the incidence of post-operative entropion.17
Biologic materials offer the potential advantages of improved incompatibility, but come at the cost of donor-site morbidity. In contrast, synthetic grafts have historically been associated with higher rates of implant-related complications, including infection and extrusion, with the advantages of being readily available and without morbidity.
The traditional management of orbital floor fracture is by transcutaneous approach, the type of surgical access is chosen taking into account the location and size of the fracture and the surgeon’s preference and experience. Another option is the endoscopic approach with minimal manipulation of the globe17. There are different methods of fracture fixation, use of porous polyethylene sheeting or titanium mesh that is fixed with one or two screws just behind the anterior border of the orbit. In children under 8 years of age, an autogenous bone graft or absorbable material should be used to accommodate the growth of the orbital skeleton17.
Implant-associated infections include implant migration, infection, exposure, palpation or local inflammatory reaction. Serious complications include post-operative optic neuropathy, blindness, and retrobulbar hematoma. Although rare, they should be discussed in detail with each patient and treatment plans should be individualized to minimize risks and maximize outcomes.
Conclusion
In our experience with the case presented, early evaluation and admission for surgical management following the international indications mentioned above are of great interest. This technique of combined material presented good results in our management as well as an adequate evaluation of the patient in the post-surgical period.
Funding
The authors declare that they have not received funding for this study.
Conflicts of interest
The authors declare that they have no conflicts of interest.
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consent. The authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Use of artificial intelligence for generating text. The authors declare that they have not used any type of generative artificial intelligence for the writing of this manuscript, nor for the creation of images, graphics, tables, or their corresponding captions.