Introduction
The posterior approach to the lumbar spine, at the level of the midline, is the best-known technique and the one that is most frequently used since it achieves the exposure of the spinous processes, the laminae, the facet joints, and the pedicles, as well as the spinal canal with its elements and intervertebral disc with the possibility of approaching the lateral portion of the vertebral bodies1,2. The ideal size is 1.5 inches per level2, and the length of the incision depends on the number of spaces to be explored1. In 1916, Esberg describes the lumbar approach without specifying the size of the incision on the wound: ”the incision is made over the spines and rapidly deepens on one side of the spinous processes, and it is generally necessary to remove the arches at least over three vertebrae to obtain sufficient exposure. As we have seen, the size of the wound in traditional approaches of spinal surgery is not at a disadvantage as MIS techniques have been made known, it can be considered in relation to the benefit over the vision that it offers for surgeons, as well as shorter radiation exposure time”3. To reduce the size of the wound, muscle trauma, bleeding, postoperative pain, and shorter hospital stay, new techniques have been developed4,5. In 1977, Williams described lumbar microdiscectomy for the treatment of herniated disc, in which he reported a reduction of the incision of the approach to 2.5 cm per level with the use of a microscope6. Gotfryd et al. performed a meta-analysis, in which the advantages of the minimally invasive, endoscopic, and standard techniques were compared, in terms of hospital stay, bleeding, and surgical efficacy7; however, the size of the wound has not been considered.
For this reason, a search was made from the medical literature in classic books, PubMed, Ovid, Cochrane, and Google Scholar; With the terms “posterior lumbar approach + wound size + incision” and “posterior lumbar approach + incision wound size”, only 3 references were found, which do not establish the size of surgical wounds in posterior lumbar approaches.
By conducting this study, it is possible to standardize the size of the wound according to the vertebral levels of intervention.
Considering that hypothetically the surgical wounds in the lumbar spine will be 3.5-4 cm per operated level, our general objective was to know the size of the surgical wounds in conditions operated by the posterior lumbar approach.
Objective
To compare the size of surgical incisions between different approaches.
Methods
It was a retrospective study, in which the digital records of patients operated by the spine surgery department using a posterior lumbar approach from 2015 to 2017 were analyzed.
Samples of post-operative clinical photographs of patients operated through a posterior lumbar approach were obtained. This included a visible measurement scale (ruler in centimeters). The patients were grouped by diagnosis, type of surgery, and levels of intervention.
Data collection was carried out by an orthopedist who was not directly involved with the patient’s surgical procedures. The data were analyzed with the SPSS version 21 statistical package. Descriptive statistics analysis was performed for quantitative variables through measures of central tendency (mean, median, and mode) and dispersion (standard deviation, maximum values, minimum, and ranges). Qualitative variables were measured in percentages. For data with normal distribution, the comparison of means between related data was performed with the paired t-test. Qualitative variables were analyzed with Chi-square and t-test for independent samples. To contrast the differences between groups, the ANOVA test p < 0.05 was used as a significant difference. The correlation with Pearson was assessed.
We included patients of any gender and age, with BMI < 30, and with visible digital photographs of the surgical wound that had a measurement scale in cm. We excluded patients with previous lumbar spine surgery.
Results
A total of 182 patients were included. The mean age was 52.5 years (SD = 18.5); 52.75% were male and 47.25% were female patients (Fig. 1). The main diagnosis operated by posterior lumbar approach was degenerative spondylolisthesis (DS) at 24.72%, followed by narrow lumbar canal (NLC) with 20.3% and herniated disc (HD) 15.4% (Fig. 2). The wound size for an HD level was 3.00 cm and lytic spondylolisthesis (LS) was 7.89 cm. (Fig. 2). For two levels, the diagnosis of degenerative disc disease (DDD) was the lowest mean with 6 cm and the highest mean was for thoracic fracture (T-Fc) with 10.3 cm. (Fig. 2). In the category of three intervened levels, the lowest mean was obtained with the diagnosis of LS with 9.02 cm and HD with 12 cm was the highest mean (Fig. 2). In the four-level group, the lowest mean was obtained with the diagnosis of intramedullary tumor (IMT) with 8 cm and vertebral destruction (VD) was the highest mean with 15.75 cm. (Fig. 2). For five levels, only two diagnoses were obtained VD with 14.5 cm and congenital scoliosis (CS) with 16 cm (Graph 2). When analyzing the main result, the mean wound size was obtained in cm per level, and for an operating level, it was 6.64 cm with a sample of 51.09% of the population, where the main operated segment was L4-L5 (Fig. 3). For two levels, a mean size of 8.5 cm was obtained, with a sample of 32.4%, where the main segment was L4-L5 L5-S1 (Fig. 3). For three levels, the mean obtained was 9.34 cm with 9.8%, and the main segment was L3-L4 L4-L5 L5-S1 (Fig. 3). In four levels, the mean was 13.1 cm with 4.39% of the sample, with the segment L1-L2-L2-L3-L3-L4 (Fig. 3). For five levels, the mean was 15 cm of the wound size with a sample of 1.6% (Fig. 3).
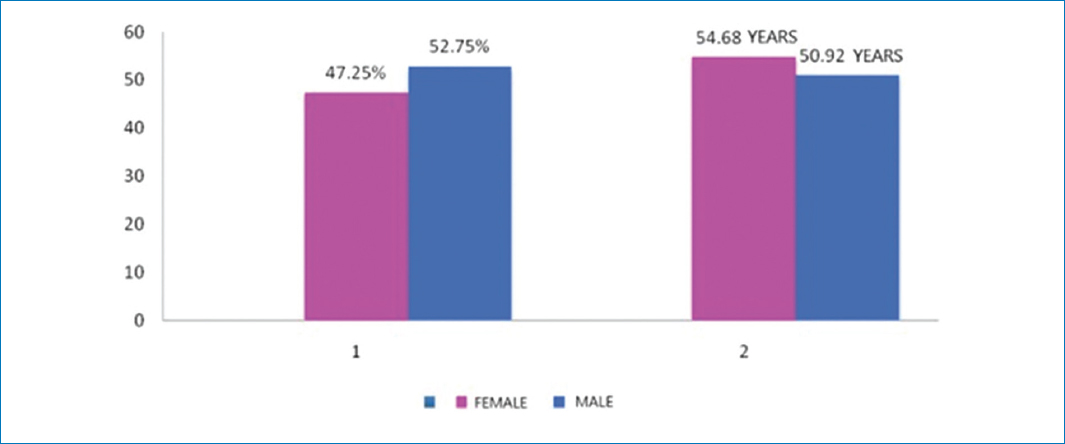
Figure 1. Sex and age.
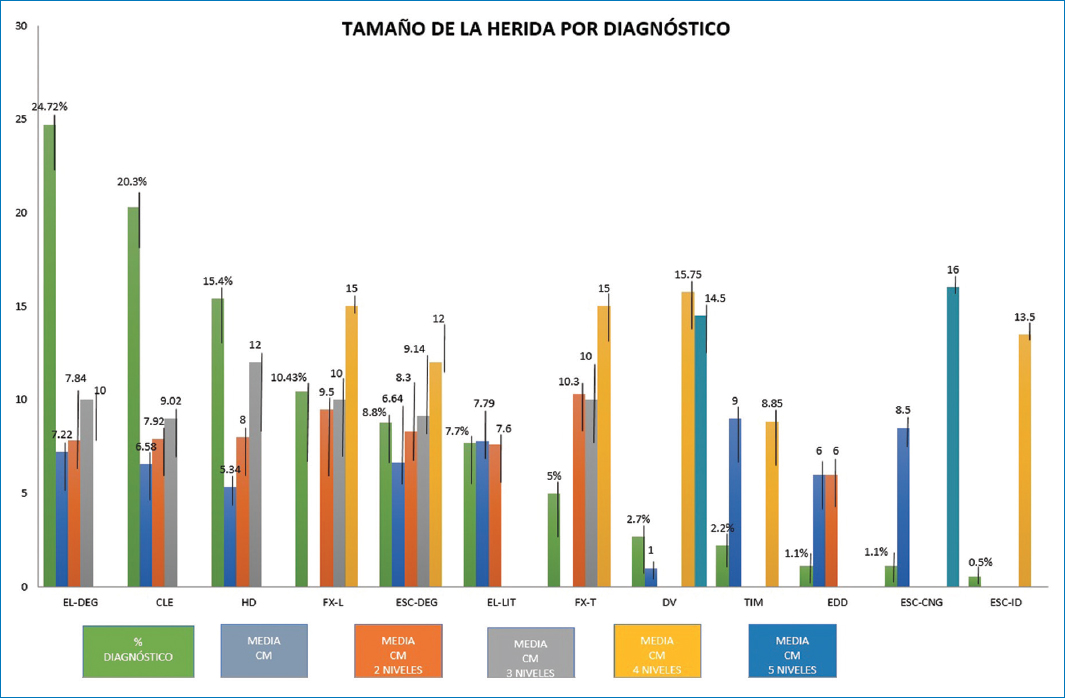
Figure 2. Wound size by diagnosis.
EL-DEG: degenerative spondylolisthesis; CLE: narrow lumbar canal; HD: herniated disc; FXL: lumbar fracture; ESC-DEG: adult degenerative scoliosis; EL-LIT: lithic spondylolisthesis; FX-T: thoracic fracture; DV: vertebral destruction; TIM: intramedullary tumor; EDD: degenerative disc disease; ESC-CNG: congenital scoliosis; ID: idiopathic scoliosis.
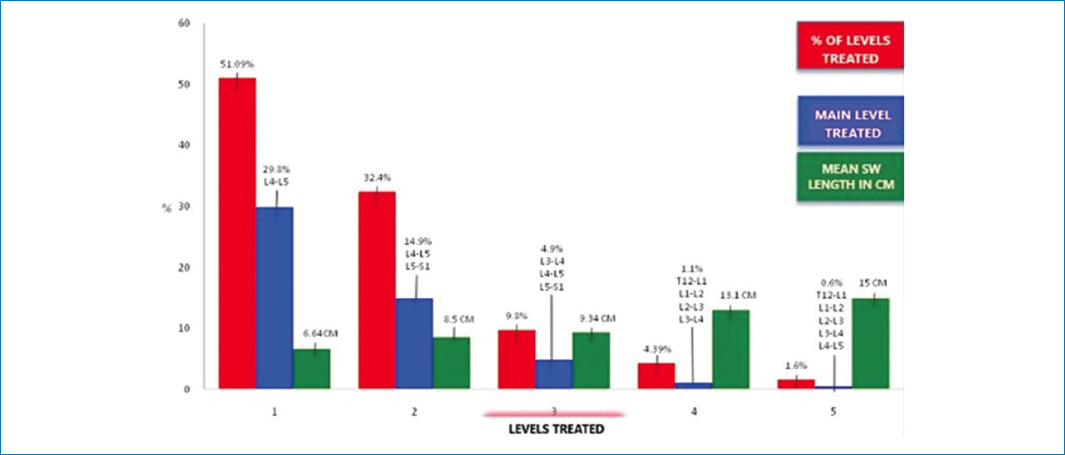
Figure 3. Mean wound length in cm by level.
When observing these results, it was considered to perform an analysis on the group of an operating level, with instrumented and non-instrumented procedures, because the mean obtained for an intervened level could be increased by this variable, for which a mean of 6.64 cm (SD = 2.083) was obtained through an N of 94, in which normal distribution was observed through a Gaussian bell (Fig. 4).
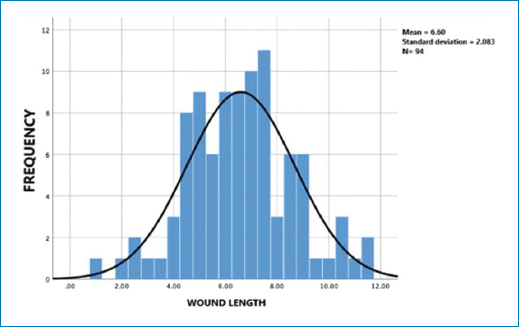
Figure 4. Gauss curve for wound length. The group that had a treated level was analyzed in relation to the instrumented and non-instrumented procedures, and the results showed a Gaussian curve with a normal distribution with a trend toward the mean.
Discussion
Currently, minimally invasive surgery systems report the size of their incisions in 2.5 cm in length per pedicle and screw8, it should be considered that this length is per side and vertebra, for which an instrumented level of L4-L5. We must consider that it is required to make four wounds of 2.5 cm each to have the same number of screws. Ulutas refers to this situation because minimally invasive systems (MIS) usually require more than one incision9. Pannu et al. refer to the 1-2 cm incision for the placement of pedicle screws per screw10. Considering, the total of incisions made, we have an approach of 4-8 cm, to this, we must consider that these systems require the use of fluoroscopy, which according to the surgeon’s experience can become excessive and has repercussions on the health status of both the surgical team and the patient.
The trend of MIS techniques is based on obtaining results with complications, shorter surgical time, short hospital stays, and less bleeding sacrificing more radiation exposure time for the surgeon and less visibility of anatomical structures. Lee et al. refer11 to a clear disadvantage of MIS in increasing radiation exposure. In 2018, Lee et al. published a study where he made a comparison between the minimally invasive versus traditional open technique in the posterior lumbar approach in the TLIF technique11, where they mention a length of 2.5 cm for the MIS approach, in the same way as its predecessors, the length of the traditional open surgery approach is not mentioned, which casts doubt on the advantage of one over the other. The size of the wound of the traditional approaches, according to the results obtained in this study, can be considered in relation to the benefit that it offers on the direct vision of the anatomical structures for the surgeons, as well as less time of radiation exposure. Tian et al.12 carried out the radiation exposure doubled compared to MIS vs. open due to the need for fluoroscopic guidance.
The mean obtained for the size of the wounds in one level surgeries was 6.64 cm, for surgeries with instrumentation; however, only for decompression, it was 3 cm. In surgeries of two or more levels, the proposed hypothesis is confirmed since the mean obtained for two levels was 8.5 cm, which gives a length of 4.25 cm for each level, in the case of three levels the mean obtained is 9.34 cm, which gives a length per level of 3.11 cm, in the case of four levels with an average of 13.1 cm, a wound size of 3.27 cm per level is obtained and for five levels with an average of 15 cm, the size is obtained per 3 cm level.
We must consider that these results are based on a single approach, for which various procedures were performed in the same incision, such as instrumentation, arthrodesis, ligamentoplasty, vertebroplasty, laminectomy, discectomy, recalibration, placement of interbody cages, among others. In this study, due to the limited literature, we only sought to obtain an average of the size of the wounds of patients operated on using the posterior lumbar approach in spinal pathologies. In perspective, the results obtained can be considered to carry out a comparative study with minimally invasive techniques and thereby establish differences between techniques.
One of the limitations of this work is considered in the lack of reference publications, to make a comparative analysis with the results obtained.
Similarly, since it is not an experimental study, it is limited to the description, and a cause–effect relationship is not established.
Conclusion
According to the results obtained, the size of the wound in traditional approaches of spinal surgery is not at a disadvantage as MIS techniques have been made known, it can be considered in relation to the benefit over the vision that it offers for surgeons, as well as shorter radiation exposure time.
In the traditional approach, only a single incision is obtained, in which most of the procedures can be performed for the spine surgeon with small surgical wounds with an adequate direct vision of work.
Funding
The authors declare that they have not received funding.
Conflicts of interest
The authors declare no conflicts of interest.
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that no patient data appear in this article. Furthermore, they have acknowledged and followed the recommendations as per the SAGER guidelines depending on the type and nature of the study.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
Use of artificial intelligence for generating text. The authors declare that they have not used any type of generative artificial intelligence for the writing of this manuscript, nor for the creation of images, graphics, tables, or their corresponding captions.