Introduction
Neonatal mortality refers to deaths occurring within the first 28 days of extrauterine life. The World Health Organization (WHO) considers it an indicator of the level of development and quality of prenatal and newborn care in a specific geographical area or health service. The perinatal period represents the most vulnerable stage for human survival and, therefore, requires high-quality care during the birthing process and newborn care1.
According to the WHO, 2.3 million newborns died worldwide in 2022, with Africa having the highest mortality rate (27 deaths/1,000 live births), followed by South Asia (21 deaths/1,000 live births). New Zealand and Australia have the lowest rates (0.7/1,000 live births)2.
The Ibero-American Society of Neonatology described in a 2011 report a significant disparity in neonatal mortality rates (NMR) among Ibero-American regions and countries. In Mexico, for example, the average national NMR is 15, ranging from 6 in some regions to 35 in others per 1,000 live births3.
The NMR in Mexico decreased from 11.6 to 7.07 deaths/1,000 live births between 1990 and 2015. The latest report from the National Institute of Statistics and Geography (INEGI, 2022) and the World Bank Group (2024) indicate a national rate of 8 deaths/1,000 births, showing little change over the last 10 years4–6.
In 2013, a study was published at this institution focusing specifically on the morbidity and mortality of premature infants exposed to tocolytics antenatally during the period from 2004 to 2008. This publication reports that 5,852 live births were registered with 25 deaths, yielding an NMR of 4.2/1,000 live births. This is the only publication offering neonatal mortality data for this hospital, although causes and ages at death are not specified7.
Recording NMR and causes of death at this hospital is crucial as it serves as an impact indicator for programs and interventions within this population and is useful for decision-making.
The objectives of this study were to determine: The early (0-7 days of life) and late (8-28 days of life) NMR in a private hospital over a 5-year period; the causes of death; and to compare the neonatal mortality of this hospital with that of other private and public hospitals nationally and internationally.
Material and methods
An observational, cross-sectional, retrospective, and descriptive clinical study was conducted. The target population included all neonates born and treated at the ABC Medical Center Santa Fe Campus from January 1, 2011, to December 31, 2015.
Inclusion criteria comprised live-born neonates of any gestational age and birth weight, whose care from birth until discharge occurred at the ABC Medical Center Santa Fe Campus. Neonates born outside the institution but treated at the ABC Medical Center Santa Fe Campus, as well as those with lost or incomplete records, were excluded.
The research protocol was reviewed and approved by the Research Committee and the Ethics Committee of the ABC Medical Center.
The method involved reviewing the digitized clinical records of all births at the ABC Medical Center, Santa Fe Campus, during the study period. Data were recorded on a data collection sheet for each patient, specifically designed to capture perinatal information, birth details, somatometry, health status, and progression in the neonatal unit. This information was later consolidated into a database.
Neonates were classified by gestational age as follows: term (37-41 weeks); late preterm (34-36 weeks); intermediate preterm (28-33 weeks); extreme preterm (< 28 weeks); and postterm (42 weeks or more). The gestational age recorded was provided by the obstetrics service, based on first-trimester ultrasound and the reliable date of the last menstrual period.
Regarding weight for gestational age, neonates were classified as follows: Appropriate for gestational age if the weight corresponded to the mean ± 2 standard deviations or fell between the 10th and 90th percentiles; small for gestational age if the weight was > 2 standard deviations below the mean or below the 10th percentile; and large for gestational age if the weight was > 2 standard deviations above the mean or above the 90th percentile, using the intrauterine growth charts accepted by NOM-007-SSA2-20168.
WHO definitions were followed for live birth, early neonatal death, late neonatal death, and NMR, as described below:
- Live birth: any neonate showing signs of life after expulsion or extraction from the mother (e.g., heartbeat, umbilical cord pulsations, breathing, or voluntary muscle movements)
- Neonatal mortality: deaths occurring within the first 28 days of life
- Early neonatal mortality: deaths occurring within the first 7 days of life
- Late neonatal mortality: deaths occurring from 7 days up to 28 days of age
- NMR: the number of neonatal deaths divided by the number of live births, expressed per 1,000 live births9–14.
Descriptive statistical analysis was performed using SPSS version 22; for qualitative variables, median, mode, minimum, and maximum ranges were utilized. For quantitative variables, mean, standard deviation, minimum, and maximum ranges were applied.
Results
Perinatal background
From 2011 to 2015, the Gynecology–Obstetrics Unit of the ABC Medical Center, Santa Fe Campus, attended 6,380 pregnant women. Of these, 6,054 (94.89%) had singleton pregnancies; 304 (4.76%) had twin pregnancies (607 newborns, including one twin pregnancy with an intrauterine fetal demise); and 22 (0.34%) had triplet pregnancies (66 newborns). A total of 6,727 live births were recorded. The median maternal age was 32.0 ± 4.6 years (16-52).
Of the 6,727 live births, 2,302 (34.22%) were vaginal deliveries, and 4,425 (65.78%) were cesarean deliveries. The cesarean delivery rate was 62.11% for singleton pregnancies, 98.35% for twin pregnancies, and 100% for triplet pregnancies.
The median gestational age of all newborns was 38.0 ± 2.0 weeks (22-42), and the median birth weight was 2,954 ± 530.78 g (450-4,712). Of the total births, 82.6% were term births and 17.4% were preterm births; 86.8% had appropriate birth weight for gestational age, and 9.3% had low birth weight for gestational age. 51.8% were male, and 48.2% were female. Table 1 shows these data and clinical conditions at discharge.
Table 1. Characteristics of newborns classified by gestational age
| Group gestational | Total (%) | Sex | Stratified weight | Condition at discharge | ||||
|---|---|---|---|---|---|---|---|---|
| Male | Female | Low birth weight | Appropriate birth weight | High birth weight | Alive | Death | ||
| Extreme preterm | 37 (0.55) | 23 (62) | 14 (38) | 11 (30) | 26 (70) | 0 (0) | 25 (67.6) | 12 (32.4) |
| Intermediate premature | 129 (1.9) | 78 (60) | 51 (40) | 20 (15.5) | 109 (84.5) | 0 (0) | 127 (98.44) | 2 (1.55) |
| Late premature | 1024 (15.2) | 558 (54.5) | 466 (45.5) | 283 (27.6) | 733 (71.6) | 8 (0.8) | 1021 (99.7) | 3 (0.3) |
| Term | 5,530 (82.2) | 2819 (51) | 2711 (49) | 313 (5.7) | 4967 (89.8) | 250 (4.5) | 5525 (99.9) | 5 (0.09) |
| Postterm | 7 (0.1) | 4 (57) | 3 (43) | 0 (0) | 7 (100) | 0 (0) | 7 (100) | 0 (0) |
| Total (%) | 6.727 (100) | 3,482 (51.8) | 3,245 (48.2) | 627 (9.3) | 5,842 (86.8) | 258 (3.9) | 6705 (99.67) | 22 (0.33) |
Of the total live births, 501 (7.45%) required more than initial resuscitation steps: 468 (6.96%) only bag-mask ventilation; 32 (0.488%) required endotracheal intubation in addition; one neonate (0.015%) required chest compressions and epinephrine administration in the delivery room.
Mortality
During the study period, 22 neonatal deaths occurred, resulting in an NMR of 3.27/1,000 live births (22/6,727). The early NMR was 2.52/1,000 live births (17/6,727), and the late NMR was 0.74/1,000 live births (5/6,727). Table 2 shows the number of neonatal deaths (early and late) grouped by birth weight and the overall NMR.
Table 2. Early and late neonatal mortality by birth weight at ABC Medical Center Santa Fe campus (2011-2015), n = 22
| Birth weight (g) | Alive newborn | Early neonatal death | Late mortality | Neonatal mortality total (%) |
|---|---|---|---|---|
| < 500 | 1 | 0 | 1 | 1 (100) |
| 500-999 | 31 | 6 | 1 | 7 (22.58) |
| 1000-1499 | 110 | 5 | 2 | 7 (6.36) |
| 1500-1999 | 295 | 2 | 1 | 3 (1.02) |
| 2000-2499 | 813 | 1 | 0 | 1 (0.12) |
| 2500-2999 | 2411 | 2 | 0 | 2 (0.08) |
| 3000-3499 | 2458 | 1 | 1 | 2 (0.08) |
| 3500-3999 | 563 | 0 | 0 | 0 (0.00) |
| 4000-4499 | 40 | 0 | 0 | 0 (0.00) |
| 4500 + | 5 | 0 | 0 | 0 (0.00) |
| Total | 6727 | 17 | 5 | 22 (0.327) |
|
Neonatal mortality rate = 3.27 × 1000 live births. |
||||
Of the 22 neonatal deaths, 77.3% (17/22) were male, and 22.7% (5/22) were female. Regarding age at death, 77.27% (17/22) occurred within the first 7 days of life; of these, 36.36% (8/22) occurred within the first 24 h of life, and 40.90% occurred between days 2 and 7; the remaining 22.73% (5/22) died between days 8 and 28.
NMR was 0.09% (5/5,530) for term infants, 0.29% (3/1,024) for late preterm infants, 2.32% (3/129) for intermediate preterm infants, and 37.8% (14/37) for extremely preterm infants (Table 3). In singleton births, the mortality rate was 0.21% (13/6054); in twin births, it was 1.15% (7/607); and in triplet births, it was 3.03% (2/66).
Table 3. Early and late neonatal mortality by gestational age at birth at ABC Medical Center Santa Fe campus (2011-2015), n = 22
| Gestational age | Alive newborns | Early neonatal death | Late neonatal death | Neonatal mortality total (%) |
|---|---|---|---|---|
| Extreme Preterm | 37 | 10 | 2 | 12 (32.43) |
| Intermediate Preterm | 129 | 1 | 1 | 2 (1.55) |
| Late Preterm | 1024 | 2 | 1 | 3 (0.29) |
| Term | 5530 | 4 | 1 | 5 (0.09) |
| Postterm | 7 | 0 | 0 | 0 (0.0) |
| Total | 6727 | 17 | 5 | 22 (3.27) |
|
Neonatal mortality rate = 3.27 × 1000 live births. |
||||
The leading causes of death were extreme prematurity with respiratory distress due to surfactant deficiency and perinatal asphyxia, sepsis, and complex heart disease (Tables 4 and 5). Table 6 shows the annual NMR, and figure 1 shows the trend of the NMR over the 5-year study period (2011-2015).
Table 4. Main causes of neonatal mortality at ABC Medical Center Santa Fe 2011-2015
| Diagnosis | Number of cases |
|---|---|
| Immaturity with surfactant deficiency and perinatal asphyxia | 7 |
| Sepsis | 7 |
| Complex congenital heart disease | 5 |
| Pulmonary Hypoplasia/HPP/acute renal failure/Shock | 1 |
| Mediastinal Mass/PPHN/Pneumothorax/electrical activity without Pulse | 1 |
| Non-immune hydrops | 1 |
|
PPHN: persistent pulmonary hypertension of the newborn; IRA: acute renal failure. |
|
Table 5. Causes of neonatal mortality according to gestational age
| Gestational age Group | Number of deaths | Causes | Number of cases |
|---|---|---|---|
| Term | 4 | Complex Congenital Hearth Diseases* | 3 |
| Severe Asphixia + Sepsis | 1 | ||
| Late Preterm | 3 | Complex Congenital Hearth Diseases** | 2 |
| Pulmonary Hypoplasia | 1 | ||
| Intermediate Preterm | 3 | HMD & Sepsis | 1 |
| PLR with PNPH | 1 | ||
| Non-Immune Hydrops | 1 | ||
| Extreme Preterm | 12 | HMD with various complications | 12 |
|
* Complex congenital heart diseases: Hypoplastic left heart (1), atresia of the valves and pulmonary arteries, severe tricuspid dysplasia (1); transposition of the great vessels, aortic arch atresia (1). Complex congenital heart diseases: Epstein’s anomaly (1); hypoplastic left heart (1). HMD: hyaline membrane disease; PLR: pulmonary liquid retention; PNPH: persistent neonatal pulmonary hypertension |
|||
Table 6. Neonatal mortality rate/1,000 live births by year ABC Medical Center Santa Fe Campus. 2011-2015
| Year | NMR |
|---|---|
| 2011 | 7.24 |
| 2012 | 2.35 |
| 2013 | 2.16 |
| 2014 | 3.45 |
| 2015 | 1.44 |
|
NMR: Neonatal mortality rate × 1,000 live births |
|
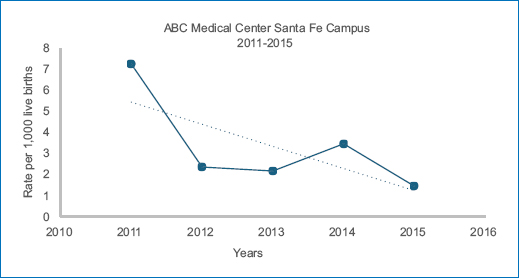
Figure 1. Neonatal mortality rate by year.
Discussion
The NMR at the ABC Medical Center maternity ward from 2011 to 2015 was 3.27/1,000 live births (Table 6 and Fig. 1). The year 2011 showed the highest NMR (7.4/1,000 live births), explained by six deaths in extremely premature infants (one weighing 450 g), two late preterm infants (one with hypoplastic lungs, the other with complex heart disease), and one term infant with complex heart disease-all incompatible with life. In 2012, the NMR decreased to 2.35; in 2013, to 2.16; in 2014, it increased slightly to 3.45; and in 2015, it decreased to 1.44/1,000 live births, demonstrating a clear downward trend. This trend is expected to continue in subsequent years.
An analysis of neonatal mortality caused by gestational age group (Table 5) reveals that in term and late preterm infants, the leading causes of death were complex heart and lung malformations, consistent with findings in other publications15,16. In intermediate and extremely premature infants, respiratory distress due to surfactant deficiency and its complications accounted for most cases, consistent with the literature15–23.
It is well known that male sex is a risk factor for neonatal morbidity and mortality. In this study, 77.3% of neonatal deaths were male, consistent with previous reports16,23.
Birth weight is a significant risk factor for death. As table 2 shows, there was only one neonate weighing < 500g who died; in those weighing between 500 g and 999 g, mortality was 22.58% (77.42% survival); between 1000 g and 1499 g, mortality decreased to 6.36% (93.64% survival); between 1500 g and 1999 g, it decreased further to 1.02% (98.98% survival); between 2000 g and 2499 g, it was 0.12% (99.88% survival); between 2500 g and 2999 g and 3000 g and 3499 g, the rate was 0.08% (99.92% survival); all infants weighing 3500 g or more survived.
Regarding gestational age, mortality was 32.43% (survival 67.57%) for those born at < 28 weeks; thereafter, mortality changed dramatically, with rates of 1.55% (98.45% survival) for those born between 28 and 33 weeks, 0.29% (99.71% survival) for those born between 34 and 36 weeks, and 0.09% (99.91% survival) for term births.
Information on the risk of death (or survival) based on birth weight and gestational age is crucial for both obstetricians and pediatricians, providing valuable data for this institution.
The number of fetuses per pregnancy also affects prognosis. In this study, the risk of death in twins was 6.5 times higher, and in triplets 13.4 times higher than in singleton pregnancies, in line with other reports24. In all cases, deaths were linked to prematurity, intrauterine growth retardation, and severe congenital malformations, implying that a higher number of fetuses exponentially increases the risk of death24–28.
Table 7 presents the NMR and leading causes of death at this hospital and other public and private hospitals with similar study periods to allow for comparison. Table 7 also includes data and references for additional hospitals.
Table 7. Comparison of neonatal mortality at ABC Medical Center Santa Fe with other private and public hospitals in the country
| Year and location; level of medical care | Total live births | Mortality rate | Mortality causes |
|---|---|---|---|
| 2011-2015 ABC Medical Center, Mexico City. Tertiary level | 6,727 1,172 (17.42%) preterm | 22 deaths 3.27 × 1000 live births | HMD with various complications, sepsis, and complex congenital heart diseases |
| 2016-2019 Ángeles de las Lomas Hospital, State of Mexico. Tertiary level17 | 4,234 584 (13.7%) preterm 57,431 | 2.7 × 1000 live births 758 deaths | HMD Neonatal sepsis Perinatal asphyxia PPHN |
| 1995-2001 General Hospital of Mexico. Tertiary level24 | 2400 (4.1%) preterm | 13.19 × 1000 | Sepsis HIV |
| February 2007-July 2008 General Hospital of Tacuba, ISSSTE. Mexico City. Second level of Care25 | 1,115 | 13 deaths 11.6 × 1000 live births | Not reported |
| 2011-2014 Mexican Social Security Institute (IMSS), Mexico. Tertiary level22 | 1,846 049 | 8.1 × 1,000 Live Births | In premature infants: Sepsis, HMD Congenital heart diseases |
| 2011-2012 General Hospital of Irapuato Second level26 | 10,532 736 (6.98%) preterm | 45 Deaths 4.2 × 1000 Live Births | No causes of death reported for term neonates |
| January 2014-August 2015 INPer, Mexico City. Tertiary level23 | 6,371 118 deaths | 118 deaths 18.5 × 1,000 live births | Congenital heart diseases |
| January 2016-January 2017 Civil Hospital of Guadalajara “Dr. Juan I. Menchaca.” Tertiary level27 | 9366 live births | 177 deaths 18.89 × 1000 live births | Malformations or genetic diseases RDS: respiratory distress syndrome Infections Hemorrhagic disorders Perinatal asphyxia |
| 1995-2012 Mariano Grajales Gynecological-Obstetric University Hospital. Cuba29 | No information | 3.8 × 1000 live births | Neonatal sepsis Congenital anomalies HMD IVH and perinatal asphyxia |
| 1998-2009 Good Samaritan Hospital, Cincinnati. Ohio USA30 | 73,547 live births | 699 deaths 11.4 × 1000 | PPHN Septicemia HIV |
|
HMD: hyaline membrane disease; IVH: intraventricular hemorrhage; PPHN: persistent pulmonary hypertension of the newborn |
|||
It is observed that in a private hospital in the State of Mexico with similar population characteristics, the NMR (during the period of 2016-2019) was 2.7/1,000 live births, with the main cause of death being hyaline membrane disease (HMD) complicated by neonatal sepsis and perinatal asphyxia17. Among public hospitals, the Hospital General de México reported an NMR of 13.19/1,000 live births in a publication covering 1995-2001, which is considered a national historical reference and surely well above its current figures; the main causes of death were persistent pulmonary hypertension in more than half of the cases, followed by septicemia and intraventricular hemorrhage18. In the Hospital General de Tacuba (ISSSTE), period 2007-2008, the reported NMR was 11.6/1,000 live births, but the causes of death were not published19. In the Mexican Social Security Institute, neonatal mortality was analyzed for 15,613 neonatal deaths that occurred from 2011 to 2014 in obstetric care hospital units across 35 delegations in 32 states of the Mexican Republic. The NMR in 2011 was 8.7, with a significant decrease in 2014 to 8.1/1,000 live births; the most frequent causes of death were prematurity and its complications, bacterial sepsis, and congenital malformations20.
At the General Hospital of Irapuato, a second-level care facility (period 2011-2012), which became a referral center with a certified NICU in 2010 for the management of preterm newborns, including those of extremely low birth weight, the reported NMR was 4.2/1,000 live births, and the main causes of death were sepsis, followed by HMD and complex congenital heart defects21.
The National Institute of Perinatology (INPer), which has a tertiary neonatal unit, reported an NMR of 17.7 in 2007 and 19.7/1,000 live births in 2008. In this study, the main causes of death were major congenital malformations incompatible with life, likely due to INPer being a high-risk maternal and neonatal referral institution15. In another more recent publication (2016) from INPer, the reported NMR was 18.5/1,000 live births and the main causes of death were extreme prematurity and complex congenital heart disease, including those who died in the same obstetric unit, with the consideration that these deaths should not be counted in the NMR as they are incompatible with life16.
In Guadalajara, a city with significant population growth and economic development, a study conducted from 2016 to 2017 at the Civil Hospital Dr. Juan I. Menchaca, which serves a low-income open population, documented an NMR of 18.8/1,000 live births, with the main causes of death being respiratory distress syndrome, infectious processes, congenital or genetic diseases, hemorrhagic disorders, and perinatal asphyxia22.
From abroad, a hospital in Cuba was selected for its excellent perinatal mortality statistics in Latin America, and a hospital in the United States was also included. At the University Gynecological–Obstetric Hospital Mariana Grajales in Cuba (period 1995-2012), the average NMR was 3.8/1,000 live births, and the most frequent causes of death were sepsis, congenital anomalies, HMD, intraventricular hemorrhage, and asphyxia29. In the Good Samaritan Hospital in Cincinnati, Ohio, USA (period 1998-2009), among 73,547 live births, the NMR was 11.4/1,000 live births; the causes of death were persistent pulmonary hypertension in newborns, septicemia, and intraventricular hemorrhage30. As can be observed, only the private hospital in the State of Mexico, which has similar characteristics in terms of the level of care and the population it serves, presents a lower NMR than this institution, albeit with a study period 5 years more recent. Regarding the main causes of death, they are very similar to those of this hospital, with slight variations.
The socioeconomic characteristics of the pregnant population served at the ABC Medical Center Santa Fe, combined with the quality of obstetric and neonatal care, as well as the technology available in both the Surgical Delivery Unit and the Neonatal Intensive Care Unit, correspond to a tertiary level of medical care. The results confirm that it is one of the best in the country, with an NMR lower than that of most hospitals in the nation and well below the national average of 8/1,000 live births, according to the latest INEGI report in 20225.
Implications for practice
According to the WHO and the International Classification of Diseases in its tenth version (ICD-10), perinatal mortality refers to deaths that occur from 22 completed weeks (154 days of gestation) until 7 days after birth. Neonatal mortality refers to newborns who die before reaching 28 days of life. These deaths are considered universal indicators of living conditions and human development, as well as quality and access to health services. To date, all health institutions include in the NMR the neonatal deaths that occur in the delivery room or birth room, and these are recorded in early neonatal mortality (the first 7 days of life). It has been proposed that these deaths occurring immediately after birth (some extend this period even to the first 6 h of life) correspond to extremely immature preterm infants or those with congenital malformations incompatible with life and should be considered in perinatal mortality (which includes deaths of neonates within the first 7 days of life) but not in early neonatal mortality, as survival does not depend on the quality of neonatal care31.
Implications for research
During the study period from 2011 to 2015, the NMR showed a clear downward trend, so it would be of great interest to conduct a new record of neonatal mortality in recent years to evaluate whether advancements in obstetric and neonatal care over the last years have had an impact and are reflected in the NMR, which should continue to decrease to the irreducible minimum.
Conclusion
Newborns continue to have different probabilities of survival worldwide based on where they are born and the accessibility and availability of health services. The NMR at the ABC Medical Center is 3.27/1,000 live births, comparable to that of other private hospitals with similar characteristics and well below the national average.
Funding
The authors declare that they have not received funding.
Conflicts of interest
The authors declare no conflicts of interest.
Ethical considerations
Protection of humans and animals. The authors declare that no experiments involving humans or animals were conducted for this research.
Confidentiality, informed consent, and ethical approval. The authors have obtained approval from the Ethics Committee for the analysis of routinely obtained and anonymized clinical data, so informed consent was not necessary. Relevant guidelines were followed.
Declaration on the use of artificial intelligence. The authors declare that no generative artificial intelligence was used in the writing of this manuscript.
