Introduction
The laparoscopic approach has become the standard of care for many abdominal surgical procedures. Compared to laparotomy, laparoscopy allows for smaller incisions, reduces the perioperative stress response, minimizes post-operative pain, and shortens recovery time1,2.
Laparoscopy relies on the establishment of a pneumoperitoneum, where a gas, typically carbon dioxide (CO2), is insufflated through the peritoneal layers to create a workspace for surgical instruments and a camera. The physiologic effects of pneumoperitoneum, CO2 absorption, and the required surgical positioning can cause physiologic disturbances, necessitating specific intraoperative care. These disturbances include changes in pulmonary function and gas exchange, which may result from increased intra-abdominal pressure (IAP) with pneumoperitoneum and from CO2 absorption. Consequently, the dynamic changes in pulmonary function during laparoscopy require intraoperative adjustments to mechanical ventilation3–5.
Conventional mechanical ventilation is a cornerstone in the management of patients under general anesthesia. However, it poses a risk of ventilator-induced lung injury (VILI), even in healthy lungs, due to the increased stress and strain imposed on pulmonary tissue. To address this, various lung protective ventilation (LPV) strategies have been proposed. LPV aims to minimize potential lung injury during ventilation, seeking the safest approach possible. Initially developed for patients with acute respiratory distress syndrome (ARDS), LPV is now frequently applied in anesthesia. This approach involves using low tidal volumes (VT) (6-8 mL/kg of predicted body weight [PBW]), positive end-expiratory pressure (PEEP), and minimizing driving pressure (ΔP)4,6,7.
Inadequate mechanical ventilation strategies during general anesthesia can lead to post-operative pulmonary complications (PPCs), especially following prolonged procedures. In the United States alone, PPCs affect approximately 1 million patients each year, resulting in an estimated 46,200 deaths and 4.8 million hospital days. These life-threatening events increase the risk of respiratory failure, atelectasis, pneumonia, pleural effusion, or pneumothorax, which may necessitate reintubation and unplanned admission to the intensive care unit (ICU). PPCs are associated with a ninefold increase in post-operative mortality6,8–10.
In 2016, the concept of mechanical power (MP) was introduced with the aim of estimating the energy delivered to the respiratory system and lungs during mechanical ventilation, measured in joules per minute (J/min). The concept quantifies the contributions of respiratory rate (RR) and PEEP to the total power delive- red by the ventilator, integrating these variables into a single measure that potentially relates to the risk of VILI. An abbreviated formula based on routine clinical data has been validated, facilitating bedside assessments in intubated patients. This concept incorporates ventilator-delivered inspiratory work, calculated from inspiratory pressures and tidal volume, as well as cyclic repetition derived from RR, enabling clinicians to assess and adjust mechanical ventilation with a single value8,11.
Research over recent years has focused on reducing PPCs by investigating how LPV interacts with surgical procedures and pneumoperitoneum. However, findings have been inconclusive, highlighting the need for a unifying concept that integrates the effects of multiple parameters when adjusting mechanical ventilation to reduce perioperative VILI.
In this study, we hypothesize that laparoscopic insufflation is associated with increased MP during intraoperative mechanical ventilation. We further investigate whether this concept provides additional insights beyond established parameters implicated in VILI, such as driving pressure, to prevent PPCs in surgical patients with healthy lungs.
Material and methods
Study design
A prospective cohort study was conducted, analyzing data from laparoscopic cholecystectomy cases performed between January 2024 and July 2024 at two academic hospitals: Centro Médico ABC Campus Observatorio and Centro Médico ABC Campus Santa Fe. Data collection, recording, and analysis focused on ventilatory parameters to describe changes in MP that may arise due to insufflation during laparoscopic surgery.
The study received approval from the institutional review boards at both institutions, which determined it met the criteria for exempt status. The requirement for informed consent was waived. A data analysis and statistical plan was established before accessing the data, which was extracted from electronic medical records, including minute-by-minute recordings of ventilator parameters.
Patient selection
Adult patients undergoing general anesthesia for laparoscopic cholecystectomy with available electronic documentation of exposure, primary outcome, and mechanical ventilation data were considered for inclusion.
Exclusion criteria included patients with a physical status of American Society of Anesthesiologists III or higher, a diagnosis of fibrotic, obstructive, or restrictive pulmonary pathology, grade III obesity, and morbid obesity. Cases with missing data for confounding varia- bles were excluded, and analyses were conducted using a complete-case approach.
During the study period (January-July 2024), a total of 204 laparoscopic cholecystectomies were performed. After applying the inclusion and exclusion criteria, 152 cases were excluded, resulting in a final study population of 52 patients. The flowchart provides a clear visualization of this selection process and has been added to the methods section to enhance transparency (Fig. 1).
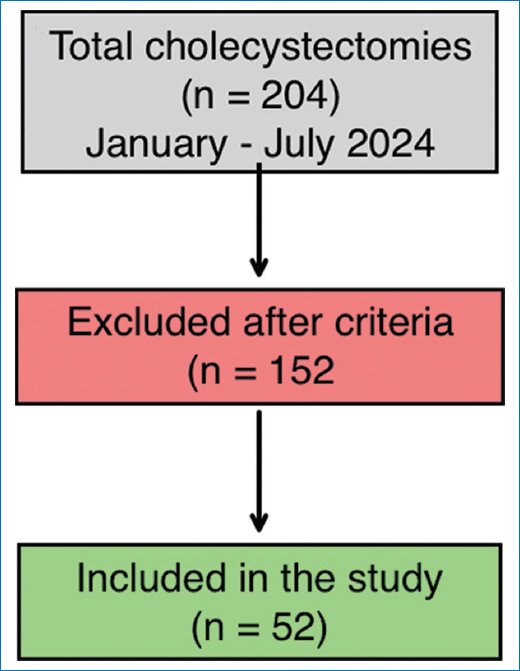
Figure 1. Flow diagram of patient selection. From a total of 204 cholecystectomies performed between January and July 2024, 152 cases were excluded based on predefined criteria. The final study sample included 52 patients.
All patients included in the study underwent laparos- copic cholecystectomy due to symptomatic gallstone disease. No patients with other indications were included, and none required additional procedures such as bile duct exploration or percutaneous drainage.
Data were collected in real time during the surgical procedure, following a predefined prospective protocol with structured recording of ventilatory variables.
Monitoring and induction
All patients were monitored according to ASA standards, including non-invasive arterial pressure measurement, capnography, oximetry, processed electroencephalogram monitoring, and electrocardiogram. Pre-oxygenation was performed with a facial mask and a fraction of inspired oxygen of 100% until an end-tidal oxygen > 90% was achieved. Intravenous induction was tailored to patient requirements and at the discretion of the attending anesthesiologist. Tracheal intubation was performed in all patients, and volume-controlled ventilation was initiated with parameters chosen by the attending anesthesiologist. Maintenance, intraoperative management, and emergence were uneventful in all cases within this cohort.
Primary analysis
Intraoperative mechanical ventilation parameters were recorded before and after pneumoperitoneum insufflation and patient positioning. The variables collected included tidal volume (Vt), RR, PEEP, plateau pressure (Pplat), peak inspiratory pressure (Ppeak), driving pressure (DP), and IAP. MP was calculated using a validated abbreviated formula for epidemiologic studies:
MP (J/min) = 0.098×RR×Vt×(PEEP+12(Pplat−PEEP)+(Ppeak−Pplat))\text{MP (J/min)} = 0.098\times\text{RR}\times \text{Vt}\times\left(\text{PEEP}+\frac{1}{2}(\text{Pplat}−\text{PEEP})+(\text{Ppeak}−\text{Pplat})\right) MP (J/min) = 0.098×RR×Vt×(PEEP+21 (Pplat-PEEP)+(Ppeak-Pplat)).
Statistical analyses
For demographic data, patients were grouped by age (≥ 60 years), body mass index (BMI) (< 25 and ≥ 25), and sex (female and male). A cutoff of 60 years was established for group division based on previous evidence indicating that age influences pulmonary mechanics and respiratory compliance, factors that can modify ventilatory response during pneumoperitoneum. Studies have reported that aging leads to a decrease in lung elasticity and thoracic compliance, which may affect the distribution of ventilatory pressures and the response to laparoscopic insufflation. In addition, this threshold has been used in previous anesthesiology and surgical studies to assess perioperative outcomes, as patients over 60 years old are at a higher risk of oxygenation disturbances and ventilatory mechanics alterations under general anesthesia.
For each category, we calculated the number of patients and the corresponding percentage. In addition, the mean and standard deviation (SD) of variables such as Vt, RR, PEEP, Pplat, Ppeak, DP, and IAP were estimated. Continuous variables were compared using either the unpaired Student’s t-test or the Mann–Whitney U test, as appropriate. Statistical significance was set at p < 0.05. All analyses were conducted using the R software, version 4.1.2.
To analyze differences between measures such as MP (pre- and post-laparoscopic insufflation), Ppeak, DP, and PP, we applied the paired Wilcoxon rank test using the “stats” package in R (R Core Team, 2021). This analysis was stratified by age, sex, BMI, and comorbidities. Similarly, the mean and SD were calculated for each category.
The paired Wilcoxon rank test was also conducted on all individuals without considering categories to assess changes in MP (pre- and post-laparoscopic insufflation) and DP. This analysis was performed using the “stats” package in R, and visualizations were created using the “ggplot2” package (Wickham, 2011).
VT across categories
Finally, the VT variable was analyzed according to the ventilator setting in mL per kg of PBW. For this analysis, an unpaired Wilcoxon rank test was conducted using the “stats” package in R. Graphs for this analysis were also created using the “ggplot2” package in R.
Results
Study cohort and characteristics
A total of 52 patients scheduled for laparoscopic cholecystectomy were included after applying the inclusion and exclusion criteria. The most relevant demographic variables, along with absolute and relative frequencies, are presented in table 1. The table also displays the mean doses used for anesthetic induction and mechani- cal ventilation parameters.
Table 1. Demographic data of the population
| Characteristic | p |
|---|---|
| Age, n (%) < 60 < 60 | 35 (67.30)17 (32.69) |
| Sex, n (%) Female Male | 34 (65.38)18 (34.61) |
| BMI, n (%) < 25 ≥ 25 | 40 (76.92)12 (23.07) |
| Comorbidity, n (%) 0 1 ≥ 2 | 22 (42.30)25 (48.07)5 (9.61) |
| Lidocaine, mean (SD) | 56.34 (21.42) |
| Propofol, mean (SD) | 130.76 (34.40) |
| Fentanyl, mean (SD) | 173.55 (44.67) |
| Pneumoperitoneum, mean (SD) | 12.11 (1.66) |
| PEEP, mean (SD) | 5.75 (0.81) |
| Respiratory rate (FR), mean (SD) | 12.63 (1.17) |
| Tidal volume (VT), mean (SD) | 427.88 (47.65) |
| Neuromuscular blocking agent, n (%) Rocuronium Cisatracurium | 48 (92.30)4 (7.69) |
| Anesthetic agent, n (%) Desflurane Sevoflurane | 27 (51.92)25 (48.07) |
|
SD: standard deviation. |
|
All patients underwent general anesthesia exclusively with the specified induction agents. Initial ventilatory parameters were recorded immediately after intubation. Surgery began with the establishment of pneumoperitoneum, with an average pressure of 12.11 mmHg (SD = 1.66). In addition, we created a histogram representing the distribution of tidal volume per kilogram of PBW, revealing a predominant use of volu- mes between 6 and 7 mL/kg PBW. Specifically, 42.3% of patients were ventilated with a tidal volume of 7 mL/kg PBW, whereas 26.9% received 6 mL/kg PBW. In addition, 21.2% were managed with 8 mL/kg PBW, and smaller proportions were observed at the extremes: 5 mL/kg PBW (3.8%) and 9 mL/kg PBW (5.8%). These findings reflect a preference for LPV strategies, with the majority of patients receiving tidal volumes within the recommended range to minimize the risk of VILI or hypoventilation (Fig. 2).
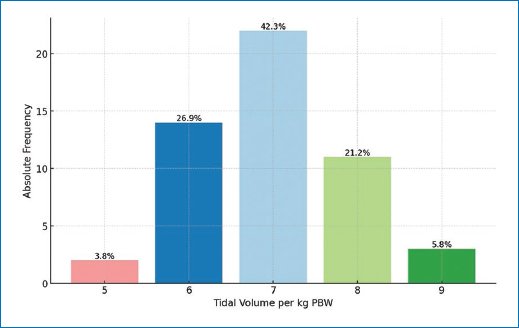
Figure 2. Distribution of tidal volume (TV) per kilogram of predicted body weight.
Significance values for the comparisons of MP-MP post, PPlateau-Plateau post, DP-DP post, and Peak-PPeak post across each of the established categories (age, sex, and BMI) are provided. Notably, all comparisons reached statistical significance, with two exceptions: the comparison of PM-PM post in the BMI (≥ 25) category (p = 0.26) and the PM-PM post comparison in patients with two or more comorbidities (p = 0.0625).
MP and driving pressure
We compared MP before and after insufflation and positioning, finding a significant increase post-insufflation (p = 9.2 × 10-7). This is reflected in the comparison of the distributions of MP and MP POST, as shown in figure 3. The box plot demonstrates that the median MP POST was higher than the median MP, with MP POST exhibiting greater variability, as evidenced by a wider interquartile range and extended whiskers. These findings indicate a broader range of MP values post-insufflation. While none of the patients in the cohort exceeded the threshold of 12 J/min of MP, the observed increase after insufflation highlights the need for caution in patients with pre-existing pulmonary pathology or low lung compliance, as these individuals may be more vulnerable to the effects of increased MP.
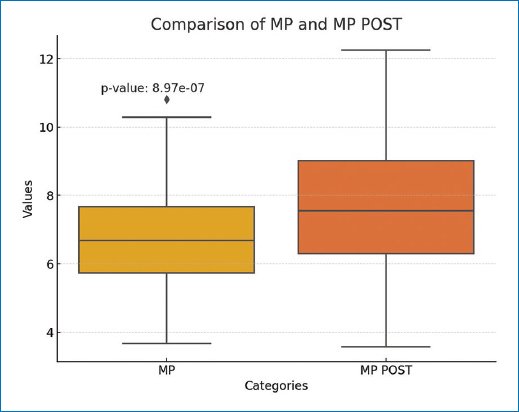
Figure 3. Boxplot comparing mechanical power before and after insufflation (MP POST). The graph illustrates the statistically significant increase in MP POST with a p value of 9.2 × 10-7, along with greater variability post-insufflation.
As part of the secondary analysis, we also compared DP values before and after insufflation and positioning. A similar trend was observed, with a significant increase in DP post-insufflation (p = 2.5e-10). In analyzing this variable, we found that some patients presented a DP > 13 cmH2O, which is currently considered the threshold for lung-protective strategies. These findings underscore the importance of adjusting mechanical ventilation following insufflation and patient positioning during laparoscopic surgery to maintain lung protection.
Subgroup analysis
AGE
Patients over 60 years of age showed significant changes between pre- and post-operative measurements across all variables (MP, PPlateau, DP, and PPeak), with p < 0.05. In this group, post-operative MP increased from 7.21 to 7.91, and PPlateau exhibited a marked rise from 13.23 to 16.88. Patients under 60 also showed significant changes in these variables, including notable increases in ventilatory pressures, such as PPeak, which rose from 16.2 to 19.45. These findings suggest that insufflation during laparoscopic surgery affects both age groups; however, older patients may be more sensitive to these physiological changes.
SEX
Both male and female patients exhibited statistically significant changes in ventilatory pressures. Women, in particular, showed a more pronounced increase in MP, rising from 6.21 to 7.54, whereas men had a higher initial MP (7.99) but experienced a less substantial post-operative change. Regarding PPlateau, women’s values increased from 13.02 to 16.41, whereas men’s values rose from 13.22 to 16.86, both with p < 0.001. Although the differences between sexes are not considerable, both groups experienced significant increases, highlighting the impact of surgery on ventilatory parameters.
BMI
Patients with a BMI ≥ 25 showed significant increases in DP (from 7.17 to 11.26) and PPeak (from 17.33 to 20), indicating a greater impact of laparoscopic surgery on the ventilatory mechanics of overweight patients. This may be attributable to reduced space for lung expansion due to increased body fat and a decrease in pulmonary compliance. In contrast, patients with a BMI < 25 also experienced significant increases in PM and DP, though the change in PPeak was smaller than in patients with higher BMI. This suggests that patients with lower BMI may better tolerate insufflation during laparoscopy, with a reduced impact on pulmonary pressures.
OVERALL FINDINGS
Across all subgroups–by age, sex, or BMI–signifi- cant increases were observed in ventilation-related variables, suggesting that laparoscopic surgery and abdominal insufflation consistently elevate respiratory pressures. These effects are likely due to diaphragm distension and compromised lung volume resulting from the surgical intervention. Total values are described in table 2.
Table 2. Population demographics divided by key variables
| Characteristic | PM | PM POST | p | PPLATEU | PPLATEU POST | p | DP | DP POST | p | PPICO | PPICO POST | p |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total population | 6.8205 | 7.6203 | 8.97e-7 | 13.0961 | 16.5 | 2.44e-10 | 7.3461 | 10.75 | 2.46e-10 | 16.423 | 19.61 | 3.5e-10 |
| Age mean (SD) | ||||||||||||
| ≥ 60 | 7.2 (1.76) | 7.91 (2.01) | 0.019 | 13.23 (2.07) | 16.88 (2.95) | 1.52e-05 | 7.23 (2.3) | 10.88 (2.71) | 0.00028 | 16.88 (2.05) | 19.94 (2.01) | 1.52e-05 |
| < 60 | 6.63 (1.63) | 7.47 (1.91) | 1.3e-05 | 13.02 (1.79) | 16.31 (2.15) | 5.82e-11 | 7.4 (1.81) | 10.68 (2.06) | 2.1e-07 | 16.2 (2.18) | 19.45 (2.75) | 2.91e-10 |
| Sex mean (SD) | ||||||||||||
| F | 6.2 (1.25) | 6.96 (1.67) | 4.4e-05 | 13.02 (1.89) | 16.41 (2.28) | 1.16e-10 | 7.44 (1.89) | 10.82 (2.11) | 3.1e-07 | 16.08 (2.17) | 19.29 (2.68) | 5.82e-10 |
| M | 7.99 (1.78) | 8.84 (1.85) | 0.0048 | 13.22 (1.86) | 16.66 (2.74) | 7.62e-06 | 7.16 (2.14) | 10.61 (2.61) | 0.00018 | 17.05 (1.98) | 20.22 (2.15) | 7.62e-06 |
| Body mass index mean (SD) | ||||||||||||
| ≥ 25 | 7.61 (2.18) | 8 (2.73) | 0.26 | 13.41 (2.35) | 17.5 (2.77) | 0.0004 | 7.17 (2.69) | 11.25 (2.73) | 0.0022 | 17.33 (1.87) | 20 (2.48) | 0.00146 |
| < 25 | 6.58 (1.44) | 7.5 (1.66) | 3.3e-07 | 13 (1.72) | 16.2 (2.26) | 1.81e-12 | 7.4 (1.73) | 10.6 (2.13) | 2.9e-08 | 16.15 (2.16) | 19.5 (2.56) | 1.81e-12 |
|
SD: standard deviation. |
||||||||||||
Statistical tests demonstrated highly significant differences, with p values well below 0.001 for most comparisons. This reinforces that the observed changes are not random, but rather a consistent response to laparoscopic insufflation.
Discussion
Our study demonstrates that laparoscopic insufflation significantly impacts ventilatory pressures, with a more pronounced effect in patients over 60 years old and those with a BMI ≥ 25. Although the literature describes a high prevalence of overweight and obesity in patients with cholelithiasis, most patients in our cohort had a normal BMI. Despite the number of patients excluded based on strict eligibility criteria, the prospective design of the study allowed for controlled confounding and consistent collection of physiological data during anesthesia. While the BMI distribution in our sample may have influenced the magnitude of the observed ventilatory changes, subgroup analyses show that patients with a BMI ≥ 25 exhibited greater increases in ventilatory pressures, suggesting higher susceptibility to mechanical alterations induced by laparoscopic insufflation. Differences by sex are less pronounced, both male and female patients exhibit meaningful changes in ventilatory parameters. Key indicators such as PPlateau and DP are critical in evaluating ventilatory mechanics during surgery; their significant post-operative increase suggests a heightened risk for developing PPCs and VILI if ventilatory management is not optimized.
MP has emerged as a promising indicator of VILI and a predictor of adverse respiratory outcomes in critically ill patients. However, few studies have explored the association between VILI and MP in low-risk patients with healthy lungs undergoing general anesthesia. The findings from our study suggest that MP could be a more reliable predictor than traditional parameters in identifying patients at risk for PPCs. Among PPCs, atelectasis is one of the most common complications, with studies indicating it can occur in up to 90% of patients undergoing general anesthesia, potentially persisting after surgery. Atelectasis in healthy lungs may result from lung parenchymal compression, gas reabsorption, small airway collapse, and surfactant dysfunction, particularly affecting lung areas near the diaphragm12–14. One of the main limitations of this study was the lack of medium- and long-term follow-up to assess the presence of post-operative lung injury. Due to the study design, a structured evaluation of respiratory complications beyond the hospitalization period was not feasible. We cannot rule out the possibility of subclinical or late effects of laparoscopic insufflation on lung function, highlighting the need for prospective studies with extended follow-up to evaluate these potential long-term effects.
Traditionally, high tidal volumes (≥ 10 mL/kg) were used to reduce atelectasis and improve oxygenation. However, high tidal volumes increase pro-inflammatory mediators, promote pulmonary edema, and lead to alveolar overdistension, contributing to lung injury and hypoxia. In contrast, low tidal volumes reduce inflammation and limit overdistension injuries but can promote atelectasis, which remains a major cause of post-operative lung injury and PPCs15.
Driving pressure (∆P) serves as an accessible surrogate for overall lung tension. Previous data show that elevated intraoperative ∆P correlates with PPCs; for instance, an observational study of nearly 70,000 patients found increased PPC odds when ∆P exceeded 12.5 cmH2O. Ahn et al. also demonstrated that driving pressure-guided ventilation (adjusting PEEP to minimize ∆P) significantly reduced PPC incidence compared to conventional ventilation in thoracic surgery. Although supporting evidence for ∆P is strong, its utility may be limited in healthy patients due to factors such as chest wall compliance, which can lead to discrepancies between ∆P and actual transpulmonary pressures, especially under conditions such as pneumoperitoneum or trendelenburg positioning16.
While driving pressure is essential, it cannot be the sole predictor of VILI. Pressure measurements alone may overestimate risk in patients with reduced chest wall compliance. Consequently, a more comprehensive, quantifiable parameter, such as MP, could offer better guidance. MP integrates key factors associated with VILI–tidal volume, RR, and driving pressure. Recent studies suggest that higher RRs contribute to PPCs, positioning RR as another critical component of MP17,18.
Our findings indicate that clinicians should monitor patients with high MP closely, identifying individuals at risk for PPCs during pre-anesthetic evaluation. Optimizing tidal volume and RR within a fixed minute volume, as per the total work equation by Otis19, and Serpa et al.20, could effectively reduce MP and the risk of VILI. The role of RR in VILI is often overlooked, with traditional guidelines focusing on maintaining end-tidal CO2 rather than the mechanical energy generated. Nevertheless, higher RRs necessitate greater flow rates, potentially increasing lung injury, as recent studies on over 100,000 patients have confirmed.
Historically, minute ventilation was increased via higher RRs to prevent hypercapnia; however, evidence increasingly supports permissive hypercapnia, which may be protective. Clinicians should limit high RRs during general anesthesia, and continuous monitoring of the flow-time curve is recommended to prevent intrinsic or auto-PEEP, which can lead to dynamic pulmonary hyperinflation and adverse hemodynamic consequences. Permissive hypercapnia achieved by reducing tidal volume or RR appears safe for low-risk patients, provided pH remains within the normal range and partial pressure of carbon dioxide elevation aligns with recommended parameters.
Our findings suggest that MP could serve as an additional biomarker alongside driving pressure to monitor dynamic lung strain. Displaying driving pressure, MP, and their trends on ventilator screens with visual safety thresholds could support clinicians in optimizing ventilation. Limiting ventilation intensity by reducing intraoperative ∆P and MP shows promise for minimizing VILI and improving patient outcomes. Although an exact “harmful” threshold for MP has yet to be defined, studies in ICU patients suggest a threshold of 12-18 J/min, with 12 J/min being generally recommended.
International guidelines derived from ARDS studies may not be fully applicable to patients with healthy lungs, as low tidal volumes could predispose them to atelectasis and PPCs. For these patients, individualized ventilatory management is recommended. We suggest using lung-protective strategies that maintain driving pressures below 15 cmH2O and intraoperative MP under 12 J/min. Patients without lung pathology may tolerate tidal volumes of 8 mL/kg with lower RRs, thus reducing MP without compromising lung protection3,4,11,21–23.
Following pneumoperitoneum establishment, higher PEEP levels may be necessary to prevent end-expiratory lung collapse. Although optimal PEEP in perioperative settings remains undefined, some evidence suggests setting PEEP at approximately 50% of IAP to optimize lung mechanics. In the absence of high-level evidence, we recommend titrating PEEP to achieve the best compliance.
Whether the association between MP and patient outcomes is primarily related to respiratory system com- pliance remains uncertain, and further randomized clinical trials are needed to validate the impact of reduced ventilatory intensity on patient outcomes. While various equations exist for calculating individual respiratory mechanics, using MP as a protective target variable in the operating room is feasible given the routine absence of transpulmonary pressure measurements.
Conclusion
Our study highlights the significant impact of laparoscopic cholecystectomy on ventilatory pressures, particularly in patients over 60 years of age and those with a BMI ≥ 25. These findings emphasize the need for vigilant monitoring and careful adjustment of mechanical ventilation parameters – especially MP and driving pressure–to minimize the risk of VILI and PPCs. As a composite metric that integrates tidal volume, RR, and pressure variables, MP may offer a more reliable indicator of lung strain than traditional parameters, even in patients without pre-existing pulmonary pathology.
We conclude that adjusting ventilation settings after pneumoperitoneum establishment, specifically by reducing MP through appropriate modifications to tidal volume, RR, and PEEP, could help optimize respiratory management in laparoscopic surgery.
Despite advances in perioperative mechanical ventilation, questions remain regarding the most effective strategies for patients undergoing laparoscopic procedures. Future research should aim to define specific thresholds for MP and evaluate the applicability of these principles across various surgical populations to improve intraoperative respiratory management. Randomized studies focusing on MP as a unifying variable for ventilation could deepen our understanding of the interactions between ventilatory parameters and surgical dynamics. This approach could lead to safer ventilation practices, reducing the incidence of PPCs and VILI in surgical patients.
Funding
The authors declare that they have not received funding.
Conflicts of interest
The authors declare that they have no conflicts of interest.
Ethical considerations
Protection of humans and animals. The authors declare that no experiments involving humans or animals were conducted for this research.
Confidentiality, informed consent, and ethical approval. The authors have followed their institution’s confidentiality protocols, obtained informed consent from patients, and received approval from the Ethics Committee. The SAGER guidelines were followed according to the nature of the study.
Declaration on the use of artificial intelligence. The authors declare that no generative artificial intelligence was used in the writing of this manuscript.
