Introduction
Idiopathic adhesive capsulitis is a disease that causes shoulder stiffness. It is characterized by gradual and painful loss of active and passive ranges of motion (ROM) of the glenohumeral joint in all planes, especially in external rotation, because of progressive fibrosis and contracture of the joint capsule1.
Adhesive capsulitis occurs in 2-5% of the population2. It occurs more frequently in women between 40 and 60 years old and is bilateral in 20-30% of cases3. It is associated with various pathological disorders such as diabetes mellitus, thyroid dysfunctions, Dupuytren’s contracture, cardiorespiratory, and autoimmune diseases4–9.
Adhesive capsulitis has been classified as primary or idiopathic and secondary. The primary is characterized by fibrosis and capsular contracture that occurs without any known triggering cause. It begins with painful and gradual restriction of the ROM of the shoulder, with no identifiable cause related to it. Secondary includes many conditions that cause shoulder stiffness, such as calcareous tendinopathy, rotator cuff tears, glenohumeral or acromioclavicular osteoarthritis, and trauma or previous shoulder or surgery10,11. The natural history of adhesive capsulitis is debatable in the literature; primary adhesive capsulitis is considered a self-limiting pathology that resolves spontaneously within 2-4 years12. However, several studies describe functional limitation, persistent pain, and weakness at long-term follow-ups13,14. Even though the pathological process often improves after these 2-4 years, pain and ROM limitation can persist indefinitely15,16.
In idiopathic adhesive capsulitis, the joint capsule is thickened and contracted with dense collagen fibers17. This results in a decrease in intra-articular volume, capsular flexibility, and glenohumeral mobility in all planes18.
Nonsurgical treatments for adhesive capsulitis include observation, physical therapy, and intra-articular steroid infiltrations19. These treatments may reduce pain but have not been shown to speed recovery20. The most commonly used treatment options include manipulation under anesthesia (MUA) and open or arthroscopic capsulotomy. Arthroscopic capsulotomy is considered more efficient and safer than MUA as it allows controlled and more complete release of the contracted capsule, thus reducing the possibility of fracture and allowing patients to obtain more immediate improvement14,21.
The restriction of external rotation was originally described as one of the characteristics of Codman’s “frozen shoulder”22. Experimental and clinical research has confirmed that contracture of the coracohumeral ligament (CHL), which limits external rotation, is the characteristic pathology of adhesive capsulitis23–26. Therefore, the release of CHL contracture and capsular thickening is fundamental in the treatment of adhesive capsulitis25.
There are very few reports about the speed of recovery in pain relief and improvement of shoulder ROM function after arthroscopic treatment of adhesive capsulitis.
The purpose of this study was to determine the immediate benefit and short-term results of arthroscopic surgery with subscapularis tendon mobilization procedure, anterior capsulotomy, and in addition, resection of the rotator interval for idiopathic adhesive capsulitis and to determine speed and degrees of functional recovery of the shoulder after this surgery. We chose to evaluate short-term recovery because there is little information available on how quickly patients recover after the procedure described above.
Patients and methods
This longitudinal and retrospective study was conducted in the Department of Orthopedics at ABC Medical Center. A review was conducted of 55 consecutive patients with a primary diagnosis of refractory idiopathic adhesive capsulitis treated with arthroscopic surgery. From this group, 51 patients with main symptoms of pain and ROM restriction, with a minimum duration of 6 months without response to medical treatment, who could meet the inclusion criteria, were analyzed. Twelve patients with rotator cuff tendon tears and four patients with evidence of glenohumeral degenerative disorders were excluded from the study. Only patients with stage II primary or idiopathic adhesive capsulitis were reviewed. This was defined by Codman’s original criteria, modified by Zuckerman et al.3,22.
The study included 39 patients (70.9%) and all were available and were able to complete the information for follow-up and analysis. All patients underwent a standardized clinical history and physical examination where symptoms and ROM were evaluated comparatively, active and passive. Health comorbidities were determined, including diabetes mellitus, thyroid disorders, and cardiovascular disease, and a history of any previous shoulder disorders was investigated. The pre-operative symptoms consisted of constant pain, prolonged evolution, progressive stiffness of the shoulder, and deterioration of activities of daily living. A predominant symptom was always nighttime pain. All patients reported insidious onset of pain after overuse, unaccustomed use, or mild trauma.
The criteria for the clinical diagnosis of idiopathic adhesive capsulitis were stiff and painful shoulder for at least 6 weeks; passive ROM restriction with loss of function and pain that disturbed sleep, making it difficult to lie on the affected shoulder. This is in the absence of other causes of pain and restriction of movement.
Pains were assessed using the Visual Analog Scale (VAS) score27. Physical examination demonstrated shoulder pain, predominantly lateral, diffuse on palpation, and often extended to the area of lateral insertion of the deltoid muscle. In addition, it was possible to demonstrate considerable restriction of ROM, active and passive. The pre-operative examination demonstrated very limited movement in all planes (Table 1).
Table 1. Pre-operative ranges of motion
| Motion | Ranges: active/passive (media) |
|---|---|
| Anterior flexion | 90°/100° |
| Abduction | 60°/70° |
| Adduction | 10°/10° |
| Extension | 10°/20° |
| External rotation in 0° | −10°/0° |
| External rotation in abduction* | 20°/20° |
| Internal rotation in abduction* | 10°/20° |
| Hand toward back | Greater trochanter (thigh ± ischium) |
|
* Possible rotation obtained. |
|
All patients presented symptoms with periods of evolution > 6 months. The average duration of shoulder pain was 11.8 months (range, 6.5-24 months) and the average duration of shoulder stiffness was 9.9 months (range, 8.5-24 months). The minimum previous treatment was 6 months (range 8-21 months), with no improvement.
Medical treatments consisted of activity modification and anti-inflammatory medication (including corticosteroids). In addition, 33 patients (84.61%) tried different physical therapy programs; 22 patients (56.41%) were treated with subacromial corticosteroid infiltration, four patients (10.25%) had hydrodilatation treatment, 46 patients (63%) were treated with non-steroidal anti-inflammatory drugs, and one patient was treated with MUA.
This study includes 11 patients (28.2%) with medication-controlled diabetes mellitus and nine patients (23%) who recalled having had “minor trauma.” All patients were in stage II (frozen stage) of the disease (marked rigidity and intense pain)17,28. We chose to include diabetic patients in the study since previous histological studies have not demonstrated differences in capsular pathology between diabetic and non-diabetic patients29.
Of the 39 arthroscopic surgeries performed on 39 patients diagnosed with idiopathic adhesive capsulitis, 25 (64.1%) were female and 14 (35.89%) were male. Twenty-four patients (61.53%) underwent surgery on the left shoulder and 15 patients (38.46%) on the right shoulder; 32 patients were right-handed and seven left-handed. Dominances were not statistically significant in clinical presentation. The average age was 52 years (35-72 years) and the follow-up period was 6 months.
Inclusion criteria
- Clinical diagnoses of stage II idiopathic adhesive capsulitis
- Symptoms with a minimum evolution of 6 months
- Minimum pre-operative medical treatment of 6 months
- Lack of response to medical treatment
- Nighttime pain
- Passive anterior elevation of < 90° and external rotation of < 30°
- Absence of other causes of pain and ROM restriction of the shoulder
- Six-month post-operative follow-up.
Exclusion criteria
- Secondary adhesive capsulitis
- Grade 2 or greater glenohumeral osteoarthritis (Kellgren-Lawrence)30
- Rotator cuff tear
- Diagnosis of rheumatoid or metabolic arthritis
- History of proximal humerus fracture
- Previous surgical treatment of the shoulder
- Period of < 6 months of evolution and medical treatment
- Post-operative follow-up of < 6 months.
Radiological analysis
Pre-operative shoulder radiographs were obtained in 31 patients (79.48%). Degrees of osteoarthritis were assessed using the Kellgren–Lawrence classification30. According to this classification, the following evaluations were obtained: 25/31 shoulders (80.64%) corresponded to grade 0 and 6/31 shoulders (19.35%) to grade 1. In addition, changes due to osteopenia were reported in 29/31 radiographs. No other evidence of pathology was demonstrated.
Magnetic resonance imaging (MRI) analysis
MRI is the most useful imaging study in patients with adhesive capsulitis. MRI scans were obtained from the shoulders of the 39 patients included in this study, which demonstrated: thickening of the CHL in 29 patients (74.35%); thickening of the anterior capsule in 37 patients (94.87%); rotator interval synovitis in 29 patients (74.35%) and increased axillary recess signal intensity in 35 patients (89%). This is directly proportional to the pain reported by patients. Muscle atrophy could also be demonstrated with fatty infiltrations of Goutallier’s grades I and II31.
In addition, MRI scans of 24 patients (61.53%) demonstrated subacromial hypertrophic bursitis and superficial fibrillation of the supraspinatus tendon, with no evidence of rupture. Intra-articular lesions were not demonstrated in any patient.
Surgical technique
Diagnostic arthroscopy was performed in a standardized sequence from the long head of the bicep’s tendon. The sites and severity of capsulitis were identified. Synovectomy and complete resection of the rotator interval were performed until the extracapsular fat and the deep surface of the coracoid process were exposed. This resection included complete resection of the CHL. This ligament represents a very important target during the surgical procedure26. Evaluations of the subscapularis tendon and overlying scar tissue showed an indurated fibrotic tissue that covered the upper surface of the subscapularis tendon and produced clear restriction of its medial and lateral displacement in 31 patients (79.48%). This fibrotic tissue was resected to expose the normal shiny transverse fibers of the subscapularis tendon surface. Biopsies of this tissue were taken from seven shoulders. Pathology results reported capsular fibrosis in four shoulders and non-specific or reactive synovitis in three shoulders. Coracoplasty was performed until a coracohumeral distance of 10 mm was obtained and the mobility of the subscapularis tendon could be completely restored. Tendon fibers were not sectioned in any case. Severe erythema with thickening and induration of the medial glenohumeral ligament was demonstrated and the ligament was resected individually in all cases. The long head of the bicep’s tendon demonstrated extensive erythema and thickening in 30 patients (76.92%); biceps tenotomy was performed in all cases. Subsequently, an anterior capsulotomy was performed, starting at the anterior glenoid rim and extending to the inferior glenoid rim. The release of the anterior structures allowed complete recovery of the external rotation of the shoulder. In none of the patients was necessary to extend the capsulotomy in the posterior direction. Research studies have shown that the extension of capsulotomy to the posterior region does not improve patient function or ROM compared to the anterior capsulotomy alone32,33. Examination of both articular surfaces demonstrated softening of the cartilage (ICRS grade 1)34.
Before completing the procedure, arthroscopy of the subacromial space was performed. Hypertrophic and fibrous bursitis was demonstrated in all shoulders. The acromion presented few osteophytes and prominence of the anterior portion of types II and III35. Partial subacromial and subdeltoid bursectomy and osteophyte resection were performed on all shoulders.
During all arthroscopies, the presumptive diagnosis of stage II idiopathic adhesive capsulitis with thickened and hyperemic tissues could be confirmed (Fig. 1). It is important to note the absence of intra-articular adhesions. No other concomitant intra-articular pathological lesions were demonstrated. At the conclusion of the procedures, all shoulders were infiltrated with a 10 mL solution of betamethasone (6 mg/mL) and ropivacaine hydrochloride (50 mg/10 mL), compression bandage was applied, and the shoulders were immobilized in a forearm sling; cryotherapy was started from the immediate post-operative period36. All patients were discharged the next day. Before hospital discharge, all patients were instructed in Codman’s pendulum exercises, in full ROM with repetitions 3-4 times a day22. It was also indicated to continue intermittent cryotherapy throughout the day.
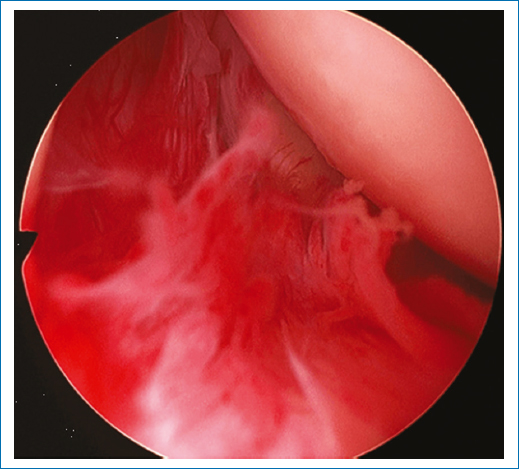
Figure 1. Adhesive capsulitis – Stage II: thickened capsular tissue with hyperemic areas in the rotator interval (right shoulder).
From the 2nd post-operative week, a standardized rehabilitation program supervised by a physical therapist was initiated. The exercises performed with the therapist were complemented by rehabilitation instructions at home, explained to each patient, and supervised during the visits. From the 6th week, patients began progressive strengthening exercises.
Patients were evaluated periodically. Follow-up visits were made at the 2nd, 6th, and 12th weeks and then patients were contacted periodically by telephone until their final evaluation at the end of the study period. Outcomes were assessed by measuring ROM, pain, and nighttime pain. All 39 patients attended follow-up visits and responded to phone calls.
Pain was assessed using the VAS score27. The pre-operative mean pain was 7.5 points. ROM was determined in both shoulders for comparison. The measurements obtained were then transformed to a value between 0 and 10 according to the Constant–Murley score to facilitate statistical analysis37,38. In addition, we evaluated the results of subjective shoulder value (SSV). Patients were asked to assign a subjective value of the affected shoulder as a comparative percentage of the value of their healthy shoulder39,40. The statistical analysis to evaluate the significance of the pre- to post-operative changes of each variable was performed using the non-parametric Wilcoxon signed rank test41. The level of statistical significance was set at p = 0.05.
Results
Varying degrees of change in the glenohumeral joint was observed in all shoulders, reflecting the diverse pathology of adhesive capsulitis28. Arthroscopy showed areas with anterior predominant capsular thickening and shrinkage in all 39 patients. Scar tissue was also observed in the subscapularis tendon and the axillary recess. In 10 shoulders (25.64%), the scar tissue deposit was distributed throughout the joint capsule. In 31 shoulders (79.48%), the indurated fibrotic tissue that covered the upper surface of the subscapularis tendon was identified. In 24 shoulders (61.53%), subacromial bursitis and acromion prominence were demonstrated with few osteophytes.
All ROM parameters improved significantly at the end of the follow-up period (p < 0.001) (Fig. 2). The mean VAS score decreased by 7.2 points compared to the pre-operative value (p < 0.001). However, most patients demonstrated very significant improvements from the 1st 8 weeks (6.5 points). Similarly, nighttime pain decreased by 8.5 points and pain with activity decreased by 7.2 points at the end of the 6-month follow-up (p < 0.001). Complaints of sleep disorder were eliminated in 36 patients (92.30%) (Fig. 3).
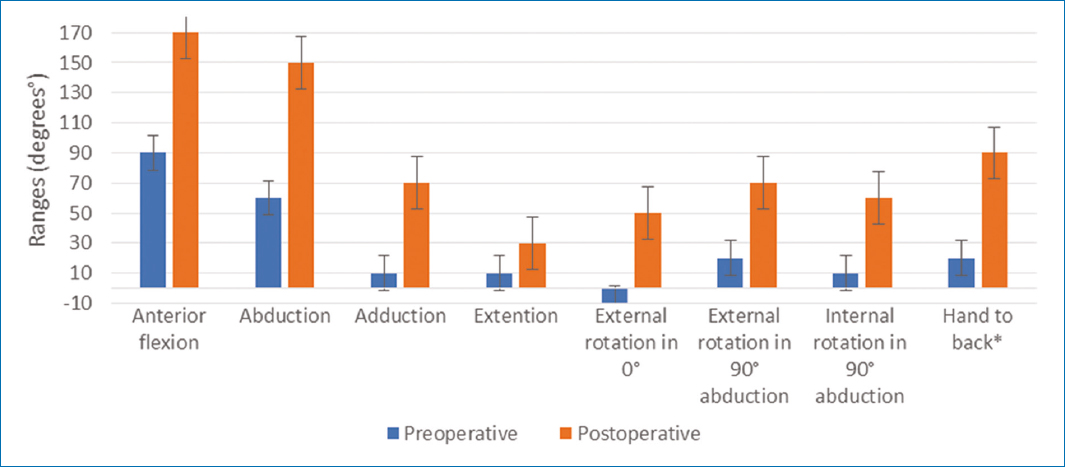
Figure 2. Pre-operative and post-operative ranges of motion (active). *Hand to back: modified from the Constant and Murley Rating Scale (@)37.
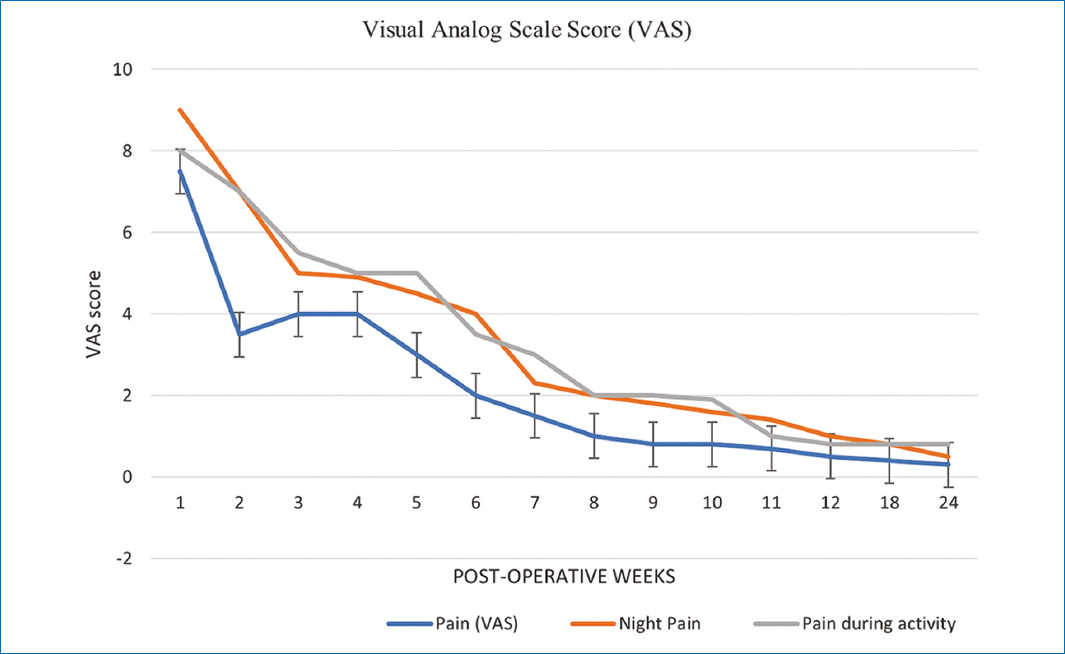
Figure 3. Average pain relief time.
All parameters improved significantly during the 1st 3 months. The SSV increased from 28% to 87% (p < 0.001). The Constant–Murley score improved in all parameters, examined, and interrogated: specifically pain, ROM, sleep disorder, SSV, and return to work and recreational activities. The final score increased from 40.3 to 86.5 points at the end of follow-up (p < 0.001). This improvement was most pronounced during the 1st 3 months and thereafter patients improved more slowly but progressively until the final follow-up (Table 2).
Table 2. Pre-operative findings and final outcome in the entire study group (n = 39)
| Measured parameters | Pre-operative values | Final result | Maximum values* | p |
|---|---|---|---|---|
| Pain* | 4.2 | 13.89 | 15 points | p < 0.0001 |
| Night pain* | 2.9 | 12.92 | 15 points | p < 0.0001 |
| Pain during activity* | 3.6 | 11.88 | 15 points | p < 0.0001 |
| Functional external rotation* | 3.87 | 8.25 | 10 points | p < 0.0001 |
| Functional internal rotation* | 3.12 | 7.33 | 10 points | p < 0.0001 |
| Work* | 1.67 | 3.58 | 4 points | p < 0.0001 |
| Recreational activities* | 1.42 | 2.99 | 4 points | p < 0.0001 |
| Sleep* | 0.35 | 1.66 | 2 puntos | p < 0.0001 |
| Use of arm in daily activities* | 4.92 | 8.48 | 10 puntos | p = 0.0003 |
| Subjective shoulder value** | 28 | 87 | 100% | p < 0.0001 |
| Constant–Murley score | 40.30 | 86.50 | 100 points | p < 0.0001 |
| Constant–Murley score (%) | 40.65 | 81.25 | 100% | p < 0.0001 |
|
* Score according to the Constant y Murley Scale44. ** Subjective Shoulder Value Value6. |
||||
Post-operative complications of arthroscopic capsulotomy are rare. The main ones include axillary nerve neuropraxia and glenohumeral instability42–45. During the post-operative period, four complications were identified: one patient developed axillary nerve neuropraxia with signs of hypoesthesia and achieved complete resolution within 6 weeks. Another patient developed a superficial anterior portal infection. He was treated with antibiotics and resolved within 2 weeks. Two normotensive patients had episodes of arterial hypertension that subsided when prednisone was discontinued, and antihypertensive medication was initiated. When comparing populations of patients who did not have complications with those who did, no significant post-operative differences were identified. There were no transoperative vascular or neurological incidents. There were no deep infections and no episodes of instability or dislocations occurred.
Discussion
The etiology of adhesive capsulitis remains uncertain; this condition is considered benign and has a self-limiting evolution22,46–50. However, its symptoms severely restrict patients’ functional, work, and sports activities and very often lead to prolonged immobilization of the shoulder51. Several research studies have shown that functional disability persists in the long term15,14,52,53. Therefore, we consider that, although the natural history of adhesive capsulitis is not well known, it is also not as benign as Codman originally suggested in 193432. Research studies have shown residual symptoms of 50%, for periods of up to 7 years, in patients treated without surgery11,16.
For a long time, it has been considered that the main pathology of adhesive capsulitis consists of the accumulation of scar tissue in the joint capsule of the shoulder3,29. Research has shown that capsular contracture and rotator interval fibrosis are the most important components of idiopathic adhesive capsulitis. The main structures affected are the CHL and the superior glenohumeral ligament. In healthy shoulders, these structures are usually elastic, and their main function is to limit excessive external rotation and inferior translation of the adducted shoulder23,26,54,55.
It is possible that the term adhesive capsulitis does not accurately reflect this pathology of the shoulder since it includes hypotheses of an inflammatory process and the presence of intra-articular adhesions. Several histological examination studies have shown that there is a minimal inflammatory response in patients with adhesive capsulitis18,29,56. Regarding adhesions, after a cadaver research study, the author stated that the axillary folds constituted the origin. Of the pathology of the so-called “frozen shoulder” and reported the “intra-articular adhesions,” which produced obliteration of the axillary recess, which gave the name to this disease3. Multiple subsequent studies have demonstrated the absence of intra-articular adhesions in adhesive capsulitis3,44,57–66. In our study, none of the 39 patients presented intra-articular adhesions or obliteration of the axillary recess.
Our study identified 39 patients with arthroscopically proven idiopathic adhesive capsulitis. The clinical diagnosis of adhesive capsulitis can be imprecise, as other conditions, such as incipient osteoarthritis and stiffness secondary to rotator cuff injuries, may mimic the symptoms. These secondary causes can only be excluded by arthroscopy as even on MRI it is very difficult to demonstrate osteoarthritis in early stages.
There is controversy about the minimum time of medical treatment, before the surgical decision, for adhesive capsulitis; this has varied between 2 and 6 months60,67–70. A research study with long-term follow-up, in untreated patients, demonstrated complete recovery in shoulder ROM in only 39% of 41 patients15. The results of another study, in a group of 62 patients with an average follow-up of 7 years, demonstrated persistence of pain and stiffness in 50% of them16.
We chose a limit of 6 months for our study since most of our patients were unwilling to continue with therapy and medication, for unpredictable times, without significant improvements, and chose surgical treatment with the aim of restoring normal function of their shoulders in less time.
Before the widespread use of arthroscopy, MUA was the standard treatment of idiopathic adhesive capsulitis. Arthroscopic capsulotomy has shown better pain relief and restoration of function, at follow-ups of 2-5 years, when compared to MUA71. The results of several studies have supported arthroscopic capsulotomy as a safe and effective treatment for idiopathic adhesive capsulitis72.
There are few arthroscopic capsulotomy studies for idiopathic adhesive capsulitis with short-term results. In our study, we demonstrated very good short-term results from the short-term as most of our patients achieved significant improvement in shoulder pain scores and ROM scores starting in the 1st 8 weeks and continued to improve until 6 months.
Posterior capsulotomy is controversial. However, although the results of some studies have shown early benefits with routine posterior capsulotomy, its longer-term results are similar to those of isolated anterior capsulotomy32,33,73. In our study, we performed only isolated anteroinferior capsulotomy because we consider that there is not enough reported evidence to justify routine posterior capsular release. Our experience has shown that this does not produce additional improvement in ROM recovery. In addition, extended capsulotomy increases surgical time and potential damage, without major additional benefits. We consider that only anteroinferior capsulotomy is required to achieve ROM recovery. Similarly, we believe that this can prevent axillary nerve injuries, especially when electrosurgical instruments or motorized instruments are used. In addition, we consider that treatment should be directed to the rotator interval and CHL contracture since this is the site of the primary pathology in idiopathic adhesive capsulitis. An additional section of the medial glenohumeral ligament and debridement of scar tissue of the subscapularis tendon produces immediate and complete external rotation. In our patient series, we were able to demonstrate a thickened CHL with gummy and highly vascularized scar tissue. The resection of the CHL and the mobilization of the subscapularis tendon in all shoulders of our series allowed us to obtain an average gain of 50° in external rotation.
Mobility of the subscapularis tendon is essential in the treatment of adhesive capsulitis. Research studies have shown thickening of the synovial membrane in the area of the rotator interval involving the superior border of the subscapularis tendon, restricting its mobility (79.80). In our study, thickened and fibrotic tissue was demonstrated that covered the superior edge of the subscapularis tendon, producing restriction of its mobility in 31 patients (79.48%). This tissue was resected to expose normal tendon fibers. In this way, enough space was created to restore the mobility of the subscapularis tendon, without requiring lengthening or section of it. The restoration of medial and lateral mobility of the subscapularis tendon was dynamically verified, without reducing the internal rotation force and allowing satisfactory recovery from external rotation.
Arthroscopic capsulotomy has also been shown to reduce pain. Results from several research studies of arthroscopic treatment with capsulotomy demonstrated significant improvement in VAS and Constant–Murley scores33,74–76. In our study, the VAS score improved from 7.5 to 0.3 and the Constant–Murley score improved from 40.30 to 86.50 and this is consistent with those studies.
An analysis of SSV showed that arthroscopic capsulotomy produces subjective improvement77,78. This is consistent with our study, whose results demonstrated an average increase of 28% to 87% of SSV in our patients.
Results from research studies of arthroscopic treatment of adhesive capsulitis have shown that subacromial decompression contributes significantly to pain relief. Several authors report significant improvement in shoulder pain in patients treated with subacromial decompression32. In our study, we demonstrated hypertrophic fibrous bursitis and few subacromial osteophytes in all 39 patients; partial, subacromial and subdeltoid, bursectomy, and osteophyte resection were performed in all shoulders. We believe that these findings could represent a secondary phenomenon of adhesive capsulitis syndrome.
It is difficult to assess the impact of intra-articular steroid injections in the literature to treat pain. However, the results of most of these studies showed that the use of steroid injections produces satisfactory results in the medium-term follow-up and little improvement in the long term53,79–81. The results of our study could suggest that intra-articular injections of betamethasone, at the end of the surgery, post-operative administration of oral prednisone, or intraoperative hydrodilatation could be the cause of the rapid improvement. However, 22 patients (56.41%) had been treated before surgery with a subacromial corticosteroid infiltration. Four patients (10.25%) had undergone hydrodilatation before surgery and several patients had taken steroids orally without any benefit. It is possible that the infiltration of prednisone influenced the improvement of pain; but we consider it unlikely that the improvement obtained, in the short term, was produced exclusively by steroids. Despite the early improvement in ROM and function, eight patients (20.51%) reported persistence of mild shoulder pain, associated with the strengthening phase of rehabilitation.
There is no consensus in the literature on the need for immobilization before the start of rehabilitation. Many authors start intensive rehabilitation immediately after surgery with daily stretching exercises32,33,79,82. Our patients kept a sling during the first 2 post-operative weeks because we considered it important to allow this period to reduce post-operative inflammation. However, Codman’s exercises were immediately initiated, and patients were instructed to discontinue the sling during periods of rest and for mild activities of daily living. Arthroscopic surgery should be continued with professional and targeted physical therapy to prevent recurrent stiffness. Our patients started a supervised rehabilitation program, and we consider that this was decisive since no patient presented recurrence.
One problem with most research studies is the sample size. It has been proposed that studies should indicate the exact stage of adhesive capsulitis in which patients are included and have an accurate diagnosis83. It has also been proposed that the investigations present surgical treatments, carried out specifically during the painful stage of adhesive capsulitis84. However, it is difficult to accurately collect and document large series of patients, during specific stages of the condition. Nonetheless, our study included 39 patients, all with stage II idiopathic adhesive capsulitis. treated with arthroscopic surgery, which included the subscapularis tendon mobilization procedure.
Validated outcome scores were used in this study3,27,37–39. Their results indicate that patients can tolerate minimal residual stiffness but what they really appreciate is the suppression or reduction of intense pain that prevents sleep. Nighttime pain is a key component of adhesive capsulitis and quite possibly one of the main indications for surgery. Before surgery, all 39 patients had been unable to sleep through the night. In our study, 92% reported that after surgery, they were able to have uninterrupted sleep between the 6th and 8th post-operative weeks. The Constant–Murley score showed similar results in diabetic patients as well.
The goal of arthroscopic treatment in shoulders with stage II adhesive capsulitis should be to shorten the natural history of the disease process and restore pain-free ROM. For an intervention to be most successful, it must produce rapid improvement, without pain, without sleep disorder, and with recovery of ROM in a short period of time since it does not have a major purpose to demonstrate improvement in 1 or 2 years, in a condition whose natural history produces subjective improvement in only 50% of patients, without any treatment, until that period27. In this study, the possibility of patients obtaining early improvement and being able to maintain it was analyzed. The majority (90%) of patients felt that their pain had significantly decreased with arthroscopic surgery during the 1st 2 weeks. Half of the patients said that their severe pain had almost disappeared within the 1st 6 weeks post-operatively.
The most important finding of this study is that, in patients who do not respond to conservative treatment of idiopathic adhesive capsulitis, mobilization of the subscapularis tendon with anteroinferior capsulotomy and resection of the rotator interval produces satisfactory improvement in pain and ROM in the short term. These findings are consistent with those reported in another study, which demonstrates that the release of the anterior capsular structures is required to restore complete ROM in a gradual manner and demonstrates the safety of the procedure and the decrease in post-operative morbidity observed in patients treated with arthroscopic surgery72. We also demonstrate that statistically significant improvements in subjective and objective parameters of shoulder function can be obtained in the short term without relevant complications.
In our review of the literature, we found a deficiency, the inclusion of mixed populations of patients with different etiologies of adhesive capsulitis (idiopathic and secondary), in most of the published series. Unlike most of these studies, ours contains only patients with idiopathic adhesive capsulitis with no history of postsurgical complications or sequelae of severe trauma. However, it is important to note that the latter may also benefit, although to a lesser extent, from the treatment described in this study.
We consider that the group of patients, defined in our study, is representative of the general population of patients with idiopathic adhesive capsulitis and we also believe that our observations are internally valid and are very possibly extensible to the general population. We attempted to minimize bias in the study design as follows: susceptibility bias was minimized by including consecutive patients and the condition was well defined to include only stage II idiopathic adhesive capsulitis. We minimized performance and execution biases as all surgeries were performed by a single surgeon with experience in arthroscopic shoulder surgery. Transfer bias was eliminated by having no patient loss rate during the study.
Our study has several strengths: it was conducted at a single Medical Center; it was possible to demonstrate satisfactory and statistically significant results, in the short term; the precise criteria for inclusion and exclusion were specified. The following were defined: stage of the disease and time of evolution of symptoms, associated with the prognosis of the treatment of idiopathic adhesive capsulitis. The entire group of treated patients was accessed. Verification of at least 6 months of pre-operative medical treatment and reduction of biases. All patients were evaluated with MRI. All patients had idiopathic adhesive capsulitis (many authors include secondary causes of shoulder capsulitis in their series) and the same surgical technique was performed in all patients. In addition, complete documentation was obtained from all patients included in the study, and validated shoulder scores were carefully used to evaluate the results. Finally, there was no loss to the follow-up rate and no missing data.
This study has several limitations: it was a retrospective analysis of data collected prospectively and without a control group to compare the results with other methods described in the literature; the outcome analysis was of a single surgeon, in a single Medical Center, and as such, may not be generalizable to a larger and more diverse group of surgeons. The results of this study cannot necessarily be extrapolated to other causes of adhesive capsulitis. Patient satisfaction data were not evaluated.
A possible criticism of this study lies in the apparent small number of patients. However, this series of 39 patients with stage II idiopathic adhesive capsulitis represents one of the largest series, as many similar reports are from groups of patients with primary and secondary capsulitis. Another criticism could be that the follow-up was short, but this is a condition that almost never recurs after improvement and this makes it unlikely that the results will deteriorate over time. Given the retrospective nature of this study, additional prospective, controlled, randomized studies are required.
Despite these limitations, we believe that the results of this study can help guide the treatment of patients with stage II idiopathic adhesive capsulitis who present with shoulder pain and stiffness. Our results demonstrate that arthroscopic surgery, with the procedures described and additional physiotherapy, produces significant and short-term symptomatic and functional improvement in patients with idiopathic adhesive capsulitis. However, the low rate of poor outcomes raises concerns about the clinical durability of the procedure. For this reason, we consider the possibility of following up this group of patients again to evaluate the long-term results of the treatment.
Conclusion
The treatment of adhesive capsulitis remains controversial despite different options and an abundance of published literature. The goal of arthroscopic treatment in shoulders with adhesive capsulitis should be to shorten the natural history of the disease process and restore pain-free ROM. For an intervention to be most successful, it must produce rapid improvement; without pain, without sleep disorder, and with ROM recovery in a period of a few weeks since it does not have much purpose to demonstrate improvement in 1 or 2 years in a condition whose natural history produces improvement in patients without treatment, until that period.
This study demonstrated that arthroscopic treatment, with mobilization of the subscapularis tendon, anteroinferior capsulotomy, and rotator interval resection, is a safe procedure that provided improvement in pain and function in all shoulders, in a shorter period than the natural history of adhesive capsulitis, thus allowing patients to recover their activity levels in the short term.
Because of the findings demonstrated in the shoulders of this study, the authors recommend paying special attention to ensuring mobility of the subscapularis tendon during arthroscopic surgery. In addition, considering that the findings demonstrated in the subacromial space may represent a secondary phenomenon of adhesive capsulitis, the authors recommend performing subacromial arthroscopy in all patients with idiopathic adhesive capsulitis.
We consider that these observations are relevant to establish indications for arthroscopic surgery in patients with adhesive capsulitis and may be useful to carry out studies with a more rigorous experimental design that compares early with late intervention to further clarify the potential benefits.
Funding
The authors declare that they have not received funding.
Conflicts of interest
The authors declare no conflicts of interest.
Ethical responsibilities
Protection of humans and animals. The authors declare that no experiments on humans or animals have been performed for this research.
Confidentiality of data. The authors declare that no patient data appear in this article.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
Use of artificial intelligence to generate texts. The authors declare that they have not used any type of generative artificial intelligence in the writing of this manuscript nor for the creation of figures, graphs, tables, or their corresponding captions or legends.
